Moxifloxacin Resistance: Why It’s Happening and How to Stop It
More people are getting sick from infections that won’t respond to moxifloxacin-not because the drug is weak, but because we’ve trained bacteria to ignore it. This isn’t science fiction. It’s happening right now in hospitals, clinics, and even in community settings across the UK and beyond. If you’ve ever been told your infection didn’t clear up after a course of moxifloxacin, you’re not alone. And the reason isn’t just bad luck-it’s a direct result of how we’ve used this antibiotic over the last two decades.
What Causes Moxifloxacin Resistance?
Moxifloxacin is a fluoroquinolone antibiotic, designed to stop bacteria from copying their DNA. That’s how it kills infections like pneumonia, sinusitis, and certain skin wounds. But bacteria don’t stay still. Every time moxifloxacin is used-especially when it’s not needed-it gives resistant strains a chance to survive and multiply.
Here’s how resistance builds:
- Overuse in humans: Doctors sometimes prescribe moxifloxacin for viral infections like colds or flu-even though antibiotics don’t work on viruses. In the UK, around 1 in 5 antibiotic prescriptions are unnecessary, according to Public Health England data from 2024.
- Incomplete courses: If you stop taking moxifloxacin once you feel better, the toughest bacteria survive. These survivors pass on their resistance genes to future generations.
- Use in agriculture: Moxifloxacin isn’t used much in farming compared to other antibiotics, but its close relatives like ciprofloxacin are. That means resistant bacteria from livestock can spread to humans through food, water, or soil.
- Genetic mutations: Some bacteria naturally develop changes in their DNA that block moxifloxacin from binding. These mutations are rare, but when antibiotics are overused, they become common.
One study from the European Centre for Disease Prevention and Control tracked moxifloxacin resistance in Streptococcus pneumoniae and found rates jumped from 2% in 2010 to over 14% in 2023 in parts of Europe. In Sheffield, local hospital labs reported a 9% rise in resistant strains between 2021 and 2024.
Why Moxifloxacin Is Different
Not all antibiotics are created equal. Moxifloxacin is broader in scope than older drugs like amoxicillin, and it’s often used as a second-line treatment when first-choice drugs fail. That makes it more valuable-and more vulnerable.
Unlike penicillin, which targets cell walls, moxifloxacin attacks DNA replication. That’s powerful-but also dangerous if misused. Bacteria can develop resistance to it through just one or two key mutations in genes like gyrA or parC. These changes are small, but they’re enough to make the drug useless.
Once resistance appears in one type of bacteria, it can spread quickly. A 2023 study in The Lancet Infectious Diseases showed that resistant strains of Mycobacterium tuberculosis carrying moxifloxacin resistance genes were found in 18% of multidrug-resistant TB cases in the UK. That’s alarming because moxifloxacin is often used in TB treatment when first-line drugs don’t work.
How to Prevent Moxifloxacin Resistance
Stopping resistance isn’t about banning moxifloxacin. It’s about using it smarter.
- Only take it when prescribed: Don’t ask for it for a sore throat unless your doctor confirms a bacterial cause. Viral infections don’t respond to antibiotics-and using them anyway adds to the problem.
- Finish the full course: Even if you feel fine after three days, keep taking it. The last 20% of bacteria are often the hardest to kill. Stopping early leaves them alive to evolve.
- Never share antibiotics: Your friend’s sinus infection isn’t the same as yours. A different bacteria, a different dose, a different risk.
- Ask about alternatives: If your doctor suggests moxifloxacin, ask: “Is this the best choice?” Sometimes amoxicillin-clavulanate or doxycycline work just as well with less risk of resistance.
- Support infection prevention: Wash your hands. Get vaccinated. Avoid close contact with sick people. Fewer infections mean fewer antibiotics needed.
Pharmacies in Sheffield have started offering free antibiotic awareness leaflets since 2023. Many now include a QR code linking to NHS guidance on when antibiotics are appropriate. These small steps matter.

What Doctors and Pharmacies Are Doing
Healthcare systems are waking up. In the UK, the NHS has rolled out Antibiotic Stewardship Programs in over 90% of hospitals. These programs require doctors to:
- Check local resistance patterns before prescribing
- Use rapid tests to confirm bacterial infections before starting antibiotics
- Document why they chose moxifloxacin over other options
Pharmacists now play a bigger role too. If you pick up a prescription for moxifloxacin, your pharmacist might ask:
- “Do you know how long to take this?”
- “Have you taken this antibiotic before?”
- “Are you experiencing any side effects like nausea or dizziness?”
These aren’t just polite questions-they’re tools to catch misuse early. A 2024 audit in Yorkshire found that pharmacist-led interventions reduced inappropriate moxifloxacin use by 22% in six months.
Solutions Beyond the Pill
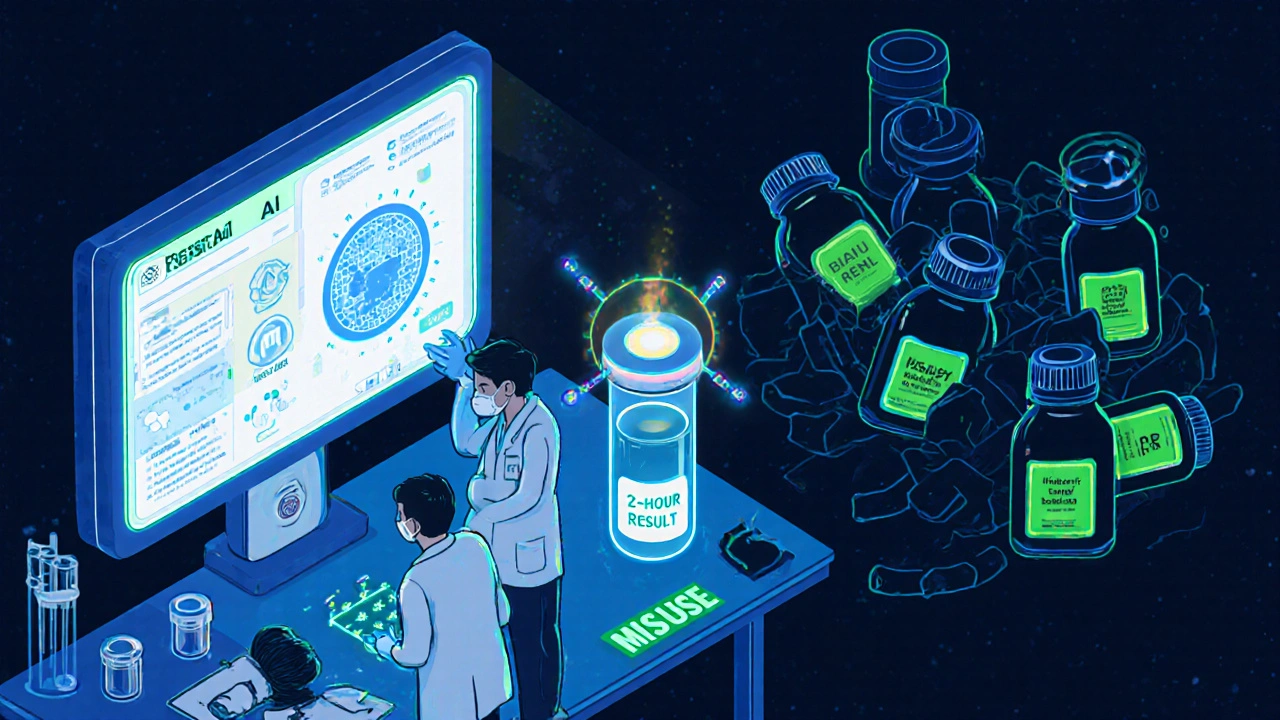
There’s no magic bullet to fix resistance. But science is exploring new paths:
- Bacteriophages: Viruses that target specific bacteria are being tested in the UK for resistant lung infections. Early trials show promise in patients who’ve run out of antibiotic options.
- Antibiotic adjuvants: New compounds like enmetazobactam can block the enzymes bacteria use to break down moxifloxacin, restoring its power.
- AI-driven diagnostics: Tools like the ResistAI platform, used in Sheffield’s Royal Hallamshire Hospital, analyze patient data and lab results to recommend the most effective antibiotic-reducing guesswork.
- Fast diagnostic tests: New PCR-based tests can identify resistant strains in under two hours instead of days. That means doctors can switch treatments faster, avoiding unnecessary moxifloxacin use.
These aren’t futuristic ideas. They’re in use now. And they’re saving lives.
What You Can Do Today
You don’t need to be a scientist to fight resistance. Here’s your action list:
- Keep a record of antibiotics you’ve taken in the last year. Share it with your doctor.
- Don’t pressure your doctor for antibiotics. Say: “I trust your judgment.”
- Dispose of leftover antibiotics properly-never flush them. Take them to your pharmacy for safe disposal.
- Support local campaigns like NHS Antibiotic Awareness Week every November.
- Teach kids about germs and hygiene. The next generation needs to grow up knowing antibiotics aren’t candy.
Resistance isn’t inevitable. It’s a choice we’ve made-repeatedly, over years. But we can choose differently.
Can moxifloxacin resistance be reversed?
Not easily, and not quickly. Once bacteria develop resistance, the genes stay in their population-even if you stop using the drug. But reducing use can lower the number of resistant infections over time. In places where moxifloxacin use dropped by 40% over three years, resistance rates fell by 15-20%. It’s slow, but it works.
Is moxifloxacin still effective for anything?
Yes-but only in the right cases. It’s still highly effective against susceptible strains of pneumonia, bacterial sinusitis, and some skin infections. The key is using it only when tests confirm the bacteria are sensitive. In hospitals, doctors now use rapid molecular tests to check before prescribing.
What happens if moxifloxacin stops working completely?
If moxifloxacin becomes useless for common infections, we lose a critical tool for treating serious illnesses like pneumonia in older adults or TB in drug-resistant cases. Patients may need longer hospital stays, more toxic drugs, or even surgery. The WHO lists fluoroquinolones like moxifloxacin as “critically important” antibiotics-losing them would push us back decades in medical progress.
Are there natural alternatives to moxifloxacin?
No. Honey, garlic, and essential oils might help with minor skin irritation, but they cannot replace antibiotics for serious bacterial infections. Relying on unproven remedies delays proper treatment and increases the risk of complications. Always consult a healthcare provider for infections that don’t improve.
How long does it take for resistance to develop?
Resistance can emerge in days if the antibiotic is misused. A 2022 study in the Journal of Antimicrobial Chemotherapy showed that after just three days of incorrect moxifloxacin dosing, resistant bacteria appeared in 30% of patients. That’s why following the prescription exactly matters more than most people realize.
Next Steps: What to Do If You’ve Had a Failed Treatment
If moxifloxacin didn’t work for you, don’t just try another antibiotic. Here’s what to do:
- Save your prescription bottle and any leftover pills.
- Write down when you started, how long you took it, and what symptoms you still have.
- Ask your doctor for a culture test-swabs or sputum samples-to identify the exact bacteria and which drugs it’s sensitive to.
- Don’t accept a new prescription without knowing why it’s better than moxifloxacin.
- Follow up in 48 hours if you’re not improving.
Every time we use an antibiotic wisely, we protect it-for ourselves, our families, and the next generation. Moxifloxacin isn’t the enemy. Misuse is. And that’s something we can change-starting today.




Comments (11)
Brittney Lopez
1 Nov 2025
Really glad someone wrote this. I had a sinus infection last year and my doctor didn’t even offer moxifloxacin right away-they asked if I’d taken antibiotics before and checked my history. Small things matter. Thanks for the clarity!
Katie Ring
2 Nov 2025
We’re not fighting bacteria-we’re fighting human arrogance. We treat antibiotics like candy because we’ve forgotten what it means to be vulnerable. This isn’t just about medicine-it’s about humility. And we’ve lost that.
Alex Sherman
3 Nov 2025
It’s amusing how casually people treat life-or-death medical tools like they’re at a grocery store. ‘Oh, I’ll just take this one because I feel kinda crummy.’ No, you won’t. You’re not a doctor. You’re not even a responsible adult. And yes, I’m talking to you, the person who saved half a pill for ‘next time.’
John Concepcion
4 Nov 2025
LMAO so now we’re supposed to trust doctors who prescribe like they’re rolling dice? And don’t get me started on pharmacists asking if I’ve taken it before-like I’m some kind of addict? I’m not a criminal for wanting to feel better. Also, ‘bacteriophages’? Sounds like sci-fi garbage. Next they’ll say we should drink bleach to kill germs.
Caitlin Stewart
4 Nov 2025
My mom used to say, ‘Don’t use a sledgehammer to crack a nut.’ That’s antibiotics in a sentence. We’ve been using a cannon for a paper cut for decades. It’s not that moxifloxacin doesn’t work-it’s that we stopped asking if we even needed it. I’ve started keeping a little log of every antibiotic I’ve taken. It’s weirdly empowering.
Emmalee Amthor
5 Nov 2025
you know what i think? we need to stop blaming people and start blaming the system. big pharma pushes these drugs like soda, doctors are rushed, and we’re left picking up the pieces. resistance isnt your fault its the system. but also-finish your pills. i know its boring but its the only thing we can control.
also i just read that some bacteria can share resistance genes like texting. like, imagine if your phone could give your friend a virus just by being near it. thats what’s happening inside us. wild.
Leslie Schnack
6 Nov 2025
Does anyone have data on how often moxifloxacin is prescribed vs. how often it’s actually needed? I’m curious if the 1 in 5 unnecessary prescriptions number includes cases where doctors were unsure and chose the broader-spectrum option just to be safe.
Saumyata Tiwari
7 Nov 2025
Of course this is a Western problem. In India, we’ve always been more cautious with antibiotics-because we’ve had to be. We don’t have the luxury of wasting drugs. Your overprescription culture is a privilege, and now you’re surprised it backfired? Classic.
Anthony Tong
9 Nov 2025
Let’s be clear: this is a manufactured crisis. The WHO and CDC have been pushing ‘antibiotic stewardship’ since the 1990s. Why? Because they want control. They want to limit access. They don’t want you to be able to treat yourself. And now they’re using fear of ‘resistance’ to justify it. You think this is about health? It’s about power.
Roy Scorer
10 Nov 2025
I’ve seen the fallout. My cousin spent three months in the hospital after a simple UTI turned into sepsis because they gave her amoxicillin first. She didn’t get moxifloxacin until it was too late. Now she’s on disability. So don’t tell me about ‘waiting’ or ‘alternatives.’ Sometimes you need the big gun. The problem isn’t the drug-it’s the delay. And the delay comes from bureaucracy, not patients.
Keerthi Kumar
11 Nov 2025
Thank you for writing this-so clearly, so gently. I’m from India, and I’ve seen how quickly antibiotics are misused here too. But I’ve also seen communities come together: school nurses teaching kids about germs, local pharmacies holding ‘Antibiotic Awareness Days’ with free testing. Change doesn’t come from laws alone. It comes from people-like you-sharing knowledge without judgment. Keep going.