Biosimilars: What They Are, How They Work, and Why They Matter
When you hear biosimilars, highly similar versions of complex biologic drugs that are not exact copies but proven to work the same way in the body. Also known as biologic generics, they offer the same clinical results as their brand-name counterparts but at a fraction of the cost. Unlike regular generic pills, which are chemically identical to their brand-name versions, biosimilars are made from living cells—so they’re more like a close cousin than a twin. This makes them harder to copy, but not impossible. The FDA and Health Canada approve them only after rigorous testing to prove they match the original in safety, purity, and strength.
Biosimilars aren’t just cheaper alternatives—they’re reshaping how we treat serious conditions like rheumatoid arthritis, Crohn’s disease, cancer, and diabetes. For example, a biosimilar to the biologic drug enoxaparin, a blood thinner used to prevent clots can cut monthly costs from $1,200 to under $300 without changing outcomes. That’s life-changing for patients on long-term therapy. And it’s not just about price. Biosimilars help stretch healthcare budgets so more people can access treatments that were once out of reach. They also push manufacturers to innovate, not just raise prices.
But not all biosimilars are created equal. Some replace older biologics with well-known safety profiles, like those used for liver transplant, a procedure requiring lifelong immunosuppression drugs. Others target newer, high-cost therapies for conditions like brain tumors, where targeted biologics can slow tumor growth. The key is knowing when a biosimilar is right for you—and when it’s not. Pharmacists use Therapeutic Equivalence Codes, FDA ratings that tell you which generics can be swapped safely to guide substitutions. But for biosimilars, the rules are stricter. You can’t just swap them like aspirin. Doctors need to approve the switch, and patients should be monitored for any unexpected reactions.
There’s still confusion out there. Some think biosimilars are "inferior" because they’re cheaper. Others worry they’re risky because they’re complex. The truth? They’re backed by years of real-world data. A 2023 study in the Journal of the American Medical Association tracked over 12,000 patients switching from brand biologics to biosimilars. No increase in side effects. No drop in effectiveness. Just savings—and more people getting the care they need.
What you’ll find below is a collection of real, practical guides on how these drugs work, who they help, and what to watch for. From biosimilars and their role in reducing drug costs to how they interact with other treatments like statins, chemotherapy, and immunosuppressants—you’ll get clear, no-fluff answers. Whether you’re a patient, caregiver, or just trying to understand your prescription, this is the kind of info that actually helps you make smarter choices.
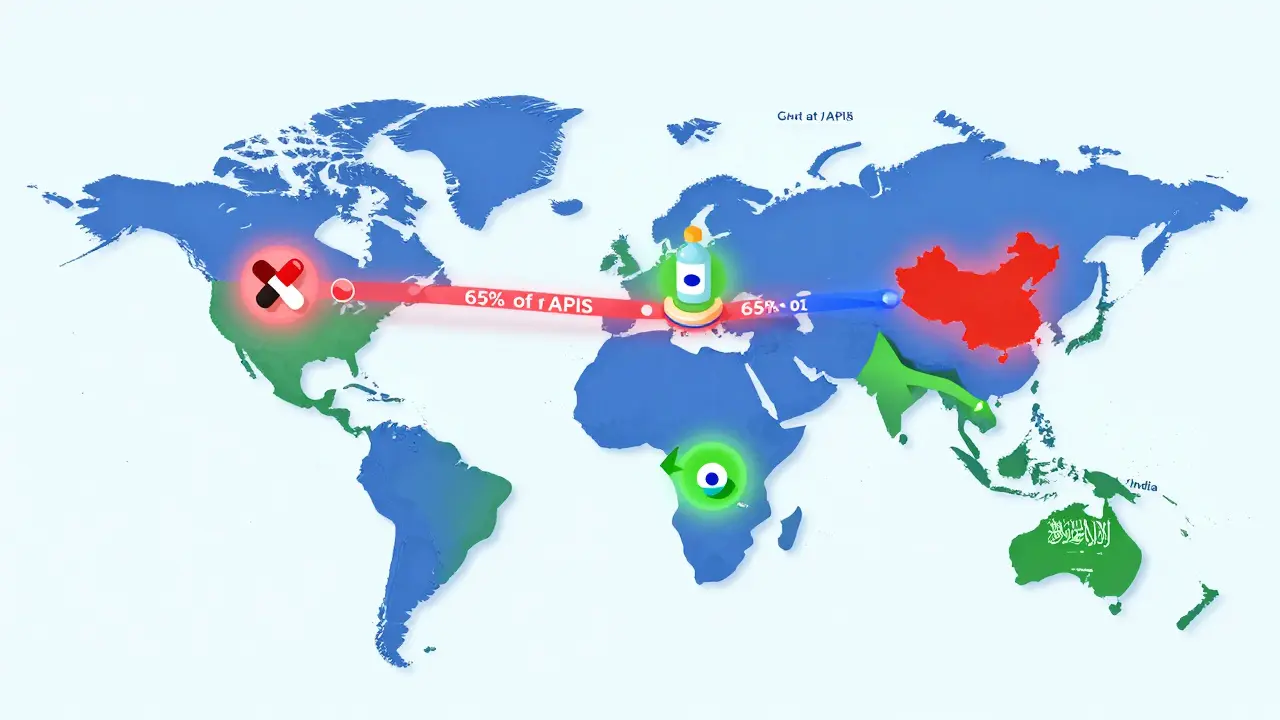
The global generic drugs market is evolving fast. With biosimilars rising, supply chains shifting, and emerging economies driving growth, affordability remains key - but quality and innovation are now just as important.
Specialty pharmacies dispense generic specialty drugs under the same strict rules as brand-name versions. Learn why cost doesn’t change the process - and how providers ensure safe, consistent care.
The global generic drug market is set to grow to over $700 billion by 2030, driven by patent expirations, aging populations, and cost pressures. Biosimilars and complex generics are leading the next wave of affordability in healthcare.