Depression Management: Practical Strategies and Medication Insights
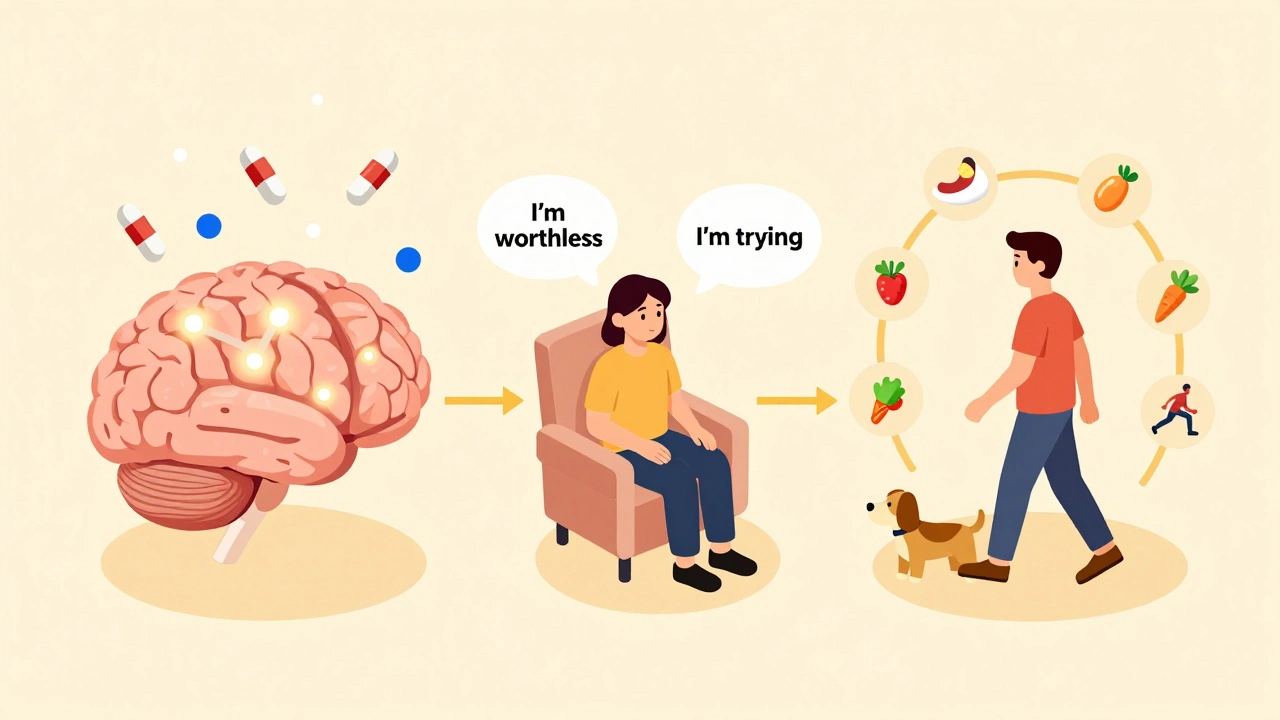
When you're dealing with depression management, the process of reducing symptoms and improving daily function through therapy, medication, and lifestyle adjustments. Also known as treating clinical depression, it's not just about popping a pill—it's about building a plan that fits your life, your body, and your needs. Many people assume depression is something you just "get over," but it’s a medical condition that often needs structured support. The right approach can turn days of exhaustion and numbness into moments of clarity and control.
One of the most common tools in depression management, the use of selective serotonin reuptake inhibitors (SSRIs) to balance brain chemistry and reduce emotional distress. Also known as antidepressants, these medications like sertraline and escitalopram are prescribed millions of times a year—not because they’re magic, but because they work for most people when used correctly. But they’re not risk-free. Side effects like nausea, sleep changes, or sexual dysfunction are common early on, and some people confuse these with allergies. That’s why knowing the difference between a side effect, an expected, non-dangerous reaction to a drug. Also known as adverse drug reaction, it's important to track what you feel and talk to your doctor before stopping anything. is key. You might be managing depression with medication, but if you’re not monitoring how your body responds, you’re flying blind.
Depression doesn’t live in isolation. It often overlaps with sleep problems, chronic pain, or other conditions like anxiety or thyroid issues. That’s why a good plan includes more than pills. Sleep hygiene, regular movement, and even how you structure your day can make a measurable difference. Some people find relief through therapy alone. Others need a combo of meds and talk sessions. And for those on multiple medications—say, for diabetes, high blood pressure, or arthritis—drug interactions become a real concern. A medication review, a scheduled check-in with a doctor or pharmacist to evaluate all current drugs for safety, effectiveness, and duplication. Also known as medication reconciliation, it's a simple step that can prevent dangerous overlaps or missed opportunities for improvement. is one of the most underused tools in mental health care. If you’re on five or more meds, you’re at higher risk for side effects that mimic or worsen depression. That’s not coincidence—it’s a system flaw.
And let’s not forget the elephant in the room: pregnancy. If you’re expecting or planning to, the question isn’t whether to take antidepressants—it’s which ones are safest and what happens if you don’t. Studies show untreated depression during pregnancy can affect both mother and baby more than SSRIs like sertraline. But you need clear, honest info—not fear-based advice. That’s why knowing the risks and benefits isn’t optional; it’s part of responsible depression management.
What you’ll find below isn’t a list of quick fixes. It’s a collection of real, practical guides written by people who’ve been there: how to tell if a reaction is an allergy or just a side effect, how to handle drug shortages that disrupt your routine, how to ask for a tier exception to save money on prescriptions, and how to prepare for a medication review that actually helps. These aren’t theory pieces—they’re tools you can use tomorrow. Whether you’re just starting out or have been managing depression for years, there’s something here that speaks to your experience—and your next step.
Depression management combines medications, therapy, and lifestyle changes based on severity. SSRIs, CBT, exercise, and sleep hygiene are evidence-backed tools. Treatment is personalized-not one-size-fits-all.