Depression Management: How Medications, Therapy, and Lifestyle Changes Work Together
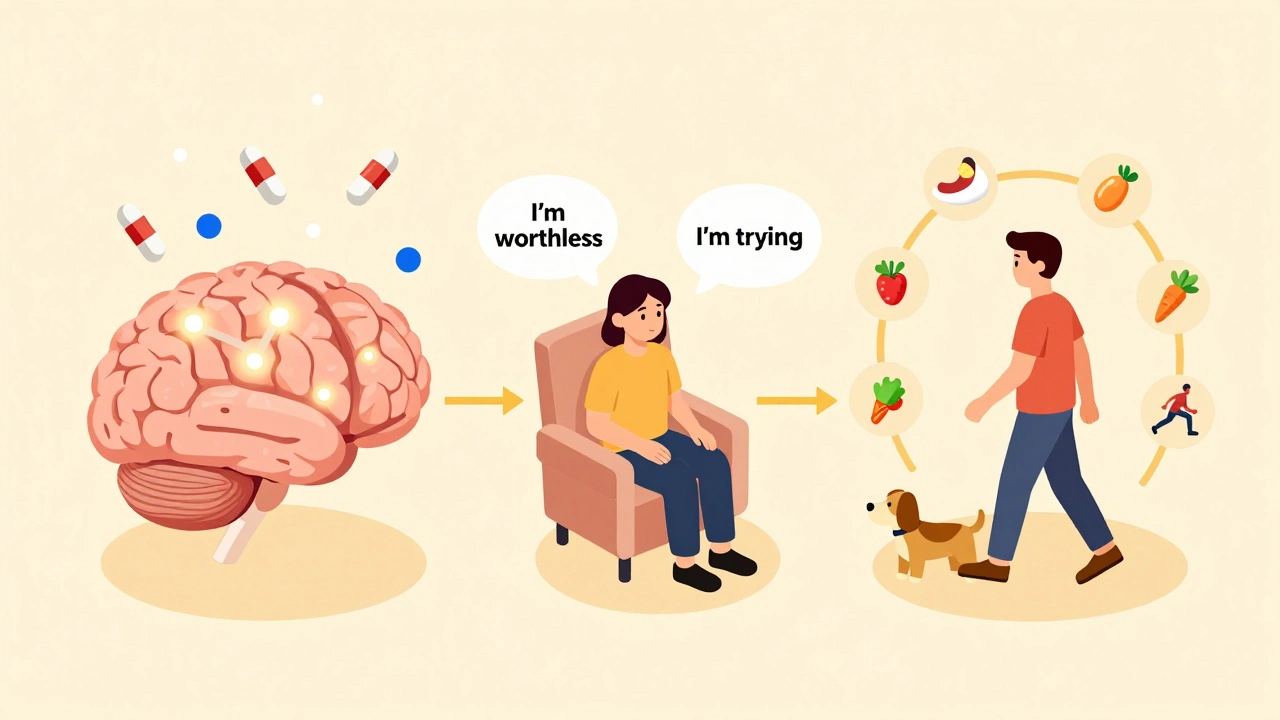
Depression isn’t just feeling sad. It’s waking up exhausted, skipping meals because food tastes like ash, and staring at the ceiling for hours because getting out of bed feels impossible. For 280 million people worldwide, this isn’t a phase-it’s a medical condition that rewires how the brain processes emotion, energy, and even basic self-care. The good news? We now have solid, science-backed ways to manage it-not just one fix, but a combination of medications, therapy, and lifestyle changes that work better together than any single approach alone.
Medications: Not a Quick Fix, But a Tool
When doctors talk about antidepressants, they’re usually referring to second-generation drugs like SSRIs (selective serotonin reuptake inhibitors). These include sertraline, citalopram, and fluoxetine. They’re not magic pills. They don’t make you happy instantly. What they do is slowly help your brain regain balance in how it handles mood-regulating chemicals. Sertraline is often the first choice because it’s affordable, well-tolerated, and backed by strong evidence.But side effects matter. About 30-50% of people on SSRIs experience sexual dysfunction. SNRIs like venlafaxine can raise blood pressure in 10-15% of users. Bupropion, on the other hand, has fewer sexual side effects but carries a small seizure risk-about 0.4% at normal doses. These aren’t random risks. They’re trade-offs. Your doctor doesn’t just pick a drug randomly. They match it to your symptoms. If you’re fatigued and sleeping too much, bupropion might help. If anxiety is your main issue, an SSRI might be better.
For mild depression, guidelines like NICE’s 2022 update say medication isn’t usually the first step. For moderate to severe cases-especially if you’re struggling to work, care for kids, or leave the house-medication becomes a key part of the plan. If two different antidepressants don’t help after 8-12 weeks each, it’s called treatment-resistant depression. Then things get more targeted: adding low-dose quetiapine can boost response rates to nearly 60%, lithium can help 36% of people who didn’t respond before, and thyroid hormone (T3) is sometimes used as an add-on. For the most severe cases, especially with psychosis or suicidal thoughts, electroconvulsive therapy (ECT) works faster and more effectively than anything else-70-90% of patients see major improvement, though memory issues can happen.
Therapy: Rewiring Thoughts, Not Just Chemicals
Medications help your brain function better. Therapy helps you understand and change how you think and act. Cognitive behavioral therapy (CBT) is the gold standard. It’s not just talking. It’s structured, goal-oriented, and backed by decades of research. In 8-28 weekly sessions, you learn to spot negative thought patterns (“I’m worthless,” “Nothing will ever get better”) and replace them with more realistic ones. Studies show CBT alone helps 50-60% of people with mild to moderate depression.Interpersonal therapy (IPT) focuses on relationships. If your depression is tied to grief, isolation, or conflict with a partner, IPT can help. Twelve to sixteen weekly sessions have shown results just as strong as medication for moderate depression. For people who’ve had depression more than once, mindfulness-based cognitive therapy (MBCT) is the go-to for preventing relapse. An 8-week group program cuts the chance of another episode by 31% over the next year.
And it’s not just individual therapy. If your depression is tied to a troubled relationship, couples therapy can be powerful. One study found 40-50% of people improved when their partner joined sessions, compared to 25-30% with individual therapy alone. The NICE guidelines specifically recommend this for people whose depression is worsened by relationship stress.
Therapy isn’t a luxury. It’s a treatment. And it’s just as effective as medication for many people. The American College of Physicians says you should pick between CBT and an antidepressant as your first step-not both, unless symptoms are severe. Why? Because starting both at once doesn’t always mean better results. It just means more cost and more effort.

Lifestyle Changes: The Foundation You Can’t Skip
No pill or therapy works well if your body is running on empty. Depression thrives on poor sleep, inactivity, and bad nutrition. The good news? Small, consistent changes can have a massive impact.Exercise isn’t just “good for you.” It’s a proven antidepressant. Three to five sessions a week of brisk walking, cycling, or swimming-30 to 45 minutes each-can be as effective as medication for mild depression. A 2020 meta-analysis found it had a standardized effect size of -0.68, which is clinically meaningful. You don’t need to run a marathon. Just move. Even a 10-minute walk outside in daylight helps reset your circadian rhythm.
Sleep is another pillar. Most people with depression have insomnia. But simply going to bed and waking up at the same time every day-even on weekends-can cut depression symptoms by 30-40%. Limit time in bed to only when you’re actually sleeping. No scrolling in bed. No naps after 3 p.m. And turn off screens an hour before bed. Blue light doesn’t just keep you awake-it disrupts melatonin, the hormone your brain needs to feel calm.
Diet matters more than most people think. The SMILES trial gave 67 people with moderate depression a 12-week Mediterranean-style diet: lots of vegetables, fruits, whole grains, fish, nuts, and olive oil. No processed food, no sugar. After 12 weeks, 32% went into remission. The control group, which got social support but no dietary changes, had an 8% remission rate. That’s not a fluke. It’s biology. Your gut and brain are wired together. What you eat affects your neurotransmitters.
Stress reduction techniques like daily mindfulness (10-20 minutes), yoga twice a week, or tai chi can lower depression scores too. These aren’t “woo-woo” practices. They’re tools that reduce cortisol, the stress hormone that gets stuck on high in depression. You don’t need to meditate for an hour. Just sit quietly, breathe, and notice your thoughts without judging them.
What Works Based on How Bad It Is
Depression isn’t one-size-fits-all. Treatment changes based on severity.- Mild depression (PHQ-9 score 5-9): Skip the meds. Start with structured exercise, guided self-help apps, or weekly check-ins with a clinician. Many people recover with just these.
- Moderate depression (PHQ-9 score 10-14): Choose either CBT or an SSRI. Both are equally effective. If you’re overwhelmed, combination therapy (therapy + medication) gives you a slightly better shot-55-60% response rate.
- Severe depression (PHQ-9 score 15+): Don’t wait. Start both medication and therapy together. Response rates jump to 60-70%. If you’re suicidal or have psychotic symptoms (delusions, hallucinations), ECT is the fastest, most reliable option.
- Chronic depression (lasting 2+ years): Standard CBT often doesn’t cut it. CBASP (Cognitive Behavioral Analysis System of Psychotherapy) is designed for this. One study found 48% of people improved with CBASP plus medication, compared to 28% with medication alone.
The key? Match the treatment to the severity. A mild case doesn’t need ECT. A severe case doesn’t need a 10-minute walk alone. That’s the “matched care” model experts now agree on.

Barriers and What’s Changing
The biggest problem isn’t lack of options-it’s access. In the U.S., only 35.6% of people with depression get any treatment. In rural areas or low-income neighborhoods, therapists are scarce. That’s why digital tools are growing fast. FDA-approved apps like reSET offer CBT-style programs and show a 47% response rate. But only 5% of clinics use them yet.Telehealth changed everything. In 2019, only 18% of therapists offered video sessions. By 2022, it was 68%. That’s huge. You can now see a therapist from your couch. You can track your mood with an app. You can join a mindfulness group online.
New treatments are coming. Psilocybin (from magic mushrooms) showed a 71% response rate in a 2021 trial, but it’s still experimental. Repetitive transcranial magnetic stimulation (rTMS)-a non-invasive brain stimulation technique-helps about half of people who didn’t respond to meds. And researchers are starting to use smartphone data-how you type, how much you move, who you text-to predict depressive episodes up to a week in advance.
But the biggest gap isn’t technology. It’s equity. Depression rates are 50% higher in racial and ethnic minority groups in the U.S., yet they’re less likely to get care. This isn’t just a medical issue-it’s a social one.
What to Do Now
If you’re struggling:- Don’t wait for it to get worse. Depression doesn’t fix itself.
- Start with one thing. Pick a daily walk. Or a 5-minute breathing exercise. Or a sleep schedule.
- Ask your doctor about CBT or an SSRI. Don’t assume medication is the only way.
- If therapy feels out of reach, try a free or low-cost app like Woebot or Moodfit.
- Remember: progress isn’t linear. Some days will feel like backsliding. That’s normal.
Depression management isn’t about fixing yourself. It’s about building a system that supports you. Medication helps your brain. Therapy helps your mind. Lifestyle changes help your body. Together, they’re not just treatments-they’re lifelines.
Can I just take medication and skip therapy?
Yes, for many people, medication alone works well-especially for moderate to severe depression. But studies show combining it with therapy leads to better long-term outcomes. Therapy teaches you skills to prevent relapse. Medication helps you get to a point where you can use those skills. If you’re only taking meds and not doing anything else, your risk of depression coming back is higher.
How long until antidepressants start working?
Most people start noticing small improvements after 2-4 weeks, but it can take 6-8 weeks to feel the full effect. Don’t stop taking them just because you don’t feel better right away. If there’s no change after 8 weeks at the right dose, talk to your doctor about switching or adding something else.
Are natural supplements like St. John’s Wort effective?
St. John’s Wort may help mild depression, but it’s not reliable for moderate or severe cases. It also interacts dangerously with many medications-including birth control, blood thinners, and other antidepressants. The FDA doesn’t regulate supplements the same way as prescription drugs. Always talk to your doctor before trying them.
What if I can’t afford therapy or medication?
Many community health centers offer sliding-scale fees based on income. Some universities train therapists who provide low-cost care. Online platforms like Open Path Collective connect people with therapists charging $30-60 per session. For medication, generic SSRIs like sertraline cost as little as $4-$10 a month in the U.S. Ask your pharmacist about patient assistance programs.
Can exercise really replace medication?
For mild depression, yes-regular exercise can be as effective as medication. But for moderate or severe depression, exercise alone isn’t usually enough. It’s best used alongside other treatments. Think of it like physical therapy after a broken leg: it helps recovery, but you still need the cast.
How do I know if I need ECT?
ECT is considered when depression is severe, life-threatening, or hasn’t responded to at least two different treatments. It’s also used for psychotic depression or when someone is too ill to eat, drink, or care for themselves. It’s not a last resort-it’s a fast, powerful tool. Side effects like temporary memory loss are common but usually improve within weeks.
Is depression curable, or will I always have it?
Depression can be managed effectively, and many people never have another episode after one treatment course. But for some, especially those with recurrent depression, it’s a condition that requires ongoing management-like diabetes or high blood pressure. The goal isn’t always to be “cured,” but to build tools and habits that keep you stable and functioning well.
If you’re reading this and feeling overwhelmed, you’re not alone. Depression lies to you. It tells you you’re broken, that nothing helps, that you’re a burden. None of that is true. Help exists. Recovery is possible. And you don’t have to do it alone.





Comments (11)
Inna Borovik
6 Dec 2025
Let’s be real-this article reads like a pharmaceutical whitepaper dressed up as self-help. The ‘lifestyle changes’ section is cute, but let’s not pretend a kale smoothie and a 10-minute walk are equivalent to neurochemical recalibration. The data here is cherry-picked to make SSRIs look like a middle ground, when in reality, the placebo response in antidepressant trials is often 30-40%. The real villain? The psychiatric-industrial complex that profits from lifelong dependency. You don’t need therapy-you need to question why your life is structured to make you miserable in the first place.
Arjun Deva
7 Dec 2025
They’re lying. All of it. SSRIs? Designed by Big Pharma to keep you docile. ECT? Mind control. The ‘Mediterranean diet’? Just a cover for GMO corn subsidies. They don’t want you cured-they want you compliant. I’ve been off meds for 7 years… and I still get flagged by my phone’s ‘mood tracking’ app. They’re watching. Always watching. And now they’re pushing ‘digital CBT’ apps to harvest your emotional data. Wake up. This isn’t treatment. It’s surveillance.
Karen Mitchell
8 Dec 2025
How dare you suggest that someone with clinical depression could possibly be helped by ‘walking outside’? This is the kind of toxic positivity that erodes real medical care. People aren’t broken because they don’t meditate enough or eat quinoa. They’re broken because society is broken. And now you’re offering them a yoga mat instead of a living wage, healthcare, or dignity. This isn’t management-it’s moralizing poverty.
Clare Fox
8 Dec 2025
what if depression isn't a problem to fix but a signal? like a fever. maybe the body's saying: this life you're living is killing you. we treat the symptom, not the cause. and then we wonder why it comes back. maybe the real treatment is quitting the job, leaving the town, saying no to the expectations. pills and therapy just help you tolerate the prison better.
Kay Jolie
9 Dec 2025
As a clinician who’s sat in 147 therapy sessions (yes, I counted), I can tell you: the real magic isn’t in the SSRIs-it’s in the therapeutic alliance. The moment someone feels *seen*, not fixed, that’s when neuroplasticity kicks in. CBT is just the scaffold. The real work? The quiet nod after you say, ‘I haven’t showered in three days.’ That’s the intervention. And yes, exercise and sleep matter-but only if you’re not too exhausted to care. Which, let’s be honest, is the whole damn problem.
Katie O'Connell
9 Dec 2025
While I appreciate the comprehensive overview, I must take issue with the conflation of efficacy with accessibility. The SMILES trial, while compelling, involved a highly controlled, nutritionally supervised cohort-hardly generalizable to populations without access to fresh produce, let alone the time and cognitive bandwidth to prepare whole foods while managing executive dysfunction. Furthermore, the article’s reliance on PHQ-9 scores as a proxy for severity is methodologically dubious; it conflates symptom frequency with existential despair. One cannot quantify the weight of inherited trauma with a Likert scale.
Nava Jothy
10 Dec 2025
OMG I’m crying rn 😭 this is the first time someone GETS it. I’ve been on sertraline for 4 years and my therapist said ‘just try yoga’ like it’s a spa day. But when I finally started walking at 6am before my kids wake up, and I ate real food and didn’t scroll for 2 hours before bed… I felt my soul come back. Not ‘cured’-but ALIVE. Thank you for saying it’s okay to need ALL of it: meds, therapy, and the quiet, lonely act of choosing to breathe.
Akash Takyar
12 Dec 2025
Thank you for this thoughtful, evidence-based piece. For those struggling in rural India, where therapists are scarce and stigma is crushing, the mention of telehealth and low-cost generics like sertraline is a lifeline. I’ve seen patients who, after six months of weekly video CBT sessions and daily walks around their village, returned to teaching school. It’s not easy. But it’s possible. And you don’t need a PhD to start: one step, one breath, one day at a time.
Mansi Bansal
13 Dec 2025
Let me tell you about my cousin. She took fluoxetine. She went to therapy. She ate kale. She meditated. She still jumped off the balcony. So tell me-what’s the point of all this ‘management’ when the system doesn’t care if you live or die? You talk about ‘matched care’ like it’s a menu. But for the poor, the brown, the queer, the traumatized-it’s a prison with a pamphlet. This article is beautiful. And it’s useless.
Jackie Petersen
14 Dec 2025
So now we’re supposed to believe that depression is just ‘bad habits’ with a fancy label? I’ve been depressed since I was 12. I didn’t choose it. I didn’t eat too much sugar. I didn’t skip yoga. My dad killed himself. My mom worked three jobs. I’m not lazy-I’m surviving. And now you want me to feel guilty because I didn’t ‘optimize’ my circadian rhythm? Screw this. I take my meds. I don’t apologize. And I won’t be shamed into ‘lifestyle changes’ by people who’ve never missed a meal because their paycheck didn’t come.
Geraldine Trainer-Cooper
14 Dec 2025
the truth is no one wants to hear that healing is boring. no epiphanies. no miracles. just showing up. even when you hate yourself. even when the sun feels like a lie. just. show. up. for the walk. for the shower. for the 3 bites of food. that’s the whole thing. no apps. no guru. no cure. just you. and the next breath.