Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): Causes, Symptoms, and What to Do
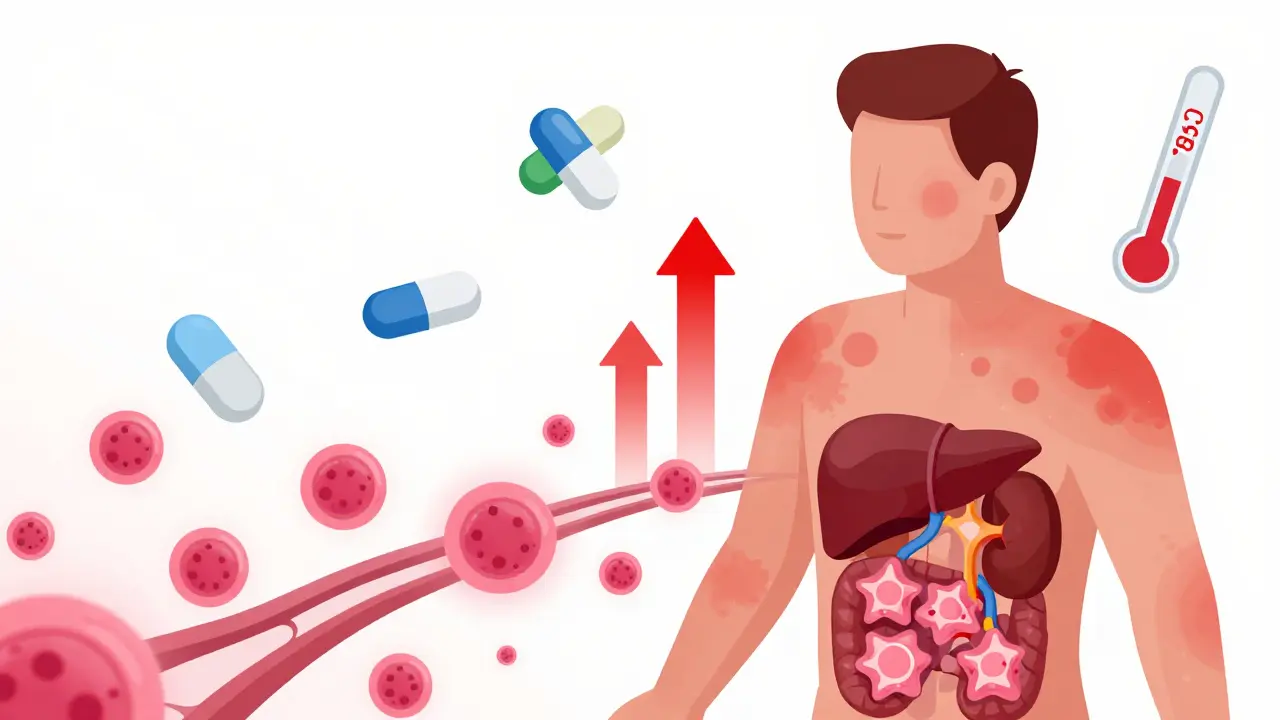
DRESS syndrome isn’t just a rash. It’s a full-body alarm triggered by a medication you thought was safe. Fever. Swollen glands. A spreading skin eruption. Liver enzymes skyrocketing. Eosinophils flooding your blood. And if you don’t catch it early, it can kill you. This isn’t a rare side effect you read about in fine print-it’s a life-threatening condition that gets missed more often than it should be. Every year in the U.S., thousands of people develop DRESS after taking common drugs like allopurinol, carbamazepine, or sulfonamides. Many don’t realize what’s happening until their organs start failing.
What DRESS Actually Looks Like
DRESS doesn’t start with a simple itchy patch. It begins quietly-like a bad cold. You feel tired. Your throat hurts. You run a fever over 38°C (100.4°F). Then, days or weeks later, the rash shows up. It’s usually red, flat, and blotchy-like measles. About 80% of cases look exactly like this. But it can also bubble, blister, or turn purple. The skin isn’t just irritated; it’s inflamed from the inside out.
What makes DRESS different from a regular drug rash? The timing. Most drug rashes appear within days of starting a new medicine. DRESS waits. It can take 2 to 8 weeks to show up. Sometimes longer. That’s why doctors often think it’s a virus, not a drug reaction. By the time they realize it’s DRESS, the damage is already spreading.
And it doesn’t stop at the skin. About 70 to 90% of patients have liver damage. ALT levels can hit over 1,000 U/L-ten times the normal range. Kidneys get hit in 10 to 30% of cases. Lungs, heart, pancreas-they’re all at risk. Blood tests show eosinophils above 1,500 per microliter. Atypical lymphocytes. High white blood cell counts. These aren’t random lab values. They’re the fingerprints of your immune system going rogue.
Which Drugs Trigger DRESS?
Not every drug causes this. But some are notorious. Allopurinol, used to treat gout, is the biggest offender. It’s responsible for 40 to 50% of all DRESS cases. That’s not a coincidence. People with kidney disease are at higher risk. If your eGFR is below 60, your chance of developing DRESS from allopurinol jumps to 1 in 200. That’s why the FDA now recommends testing for the HLA-B*58:01 gene before prescribing allopurinol to Asian patients-those with this gene have up to a 90% higher risk.
Antiepileptic drugs like carbamazepine, phenytoin, and lamotrigine come next. They cause 20 to 30% of cases. Sulfonamide antibiotics-like Bactrim-are another common trigger. Even some antivirals and NSAIDs have been linked. But here’s the catch: it’s not about the dose. It’s about your body’s reaction. Two people take the same drug, same dose. One gets a mild rash. The other goes into multi-organ failure. Why? Genetics. Immune history. Viral reactivation.
That last part is critical. In 60 to 70% of DRESS cases, the body reactivates HHV-6, a herpes virus most people carry silently. It doesn’t cause the reaction-but it makes it worse. The virus flares up 2 to 4 weeks after symptoms start, fueling inflammation and prolonging recovery. That’s why some patients seem to get better, then crash again weeks later.
DRESS vs. SJS/TEN: Why the Difference Matters
People often confuse DRESS with Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). They’re all severe drug reactions. But they’re not the same.
SJS and TEN hit fast-within 1 to 4 weeks. The skin blisters and peels off in sheets. Mucous membranes in the mouth, eyes, and genitals are destroyed. Mortality is high-up to 40% for TEN. DRESS doesn’t cause that kind of skin detachment. Instead, it attacks organs from within. The rash is less dramatic, but the internal damage is deeper and longer-lasting.
The immune systems involved are different too. SJS/TEN are driven by killer T-cells that directly destroy skin cells. DRESS is a slow-burn fire: CD4+ T-cells activate, eosinophils swarm tissues, and cytokines like IL-5 and IL-13 turn inflammation into tissue destruction. That’s why steroids work better in DRESS than in SJS/TEN.
And the outcomes? DRESS kills about 10% of people-usually from liver failure. SJS kills 5 to 10%. TEN kills 30 to 40%. But DRESS has a hidden cost: long-term autoimmune damage. About 5 to 10% of survivors develop thyroid disease, lupus, or type 1 diabetes months or even years later. One patient on Reddit developed Graves’ disease five weeks after their DRESS symptoms cleared. That’s not rare. It’s expected.

How Doctors Diagnose It (And Why It’s Often Missed)
There’s no single blood test for DRESS. Diagnosis relies on a checklist. The RegiSCAR criteria require hospitalization plus at least three of these: fever, rash, swollen lymph nodes, eosinophilia, atypical lymphocytes, and involvement of three or more organs. If you meet the criteria, it’s DRESS.
But here’s the problem: most doctors don’t know the checklist. A 2020 study found only 35% of internal medicine residents could correctly identify a DRESS case. Patients see three or more doctors before getting the right diagnosis. One patient spent six weeks in and out of ERs before a dermatologist spotted the pattern: fever + rash + high eosinophils + recent allopurinol use. That’s the key.
Doctors look for viruses. They check for mononucleosis. They treat for bacterial infections. They miss the drug connection because the timeline doesn’t fit. If you started a new medication three weeks ago and now have a fever and rash, ask: Could this be DRESS? That question saves lives.
What Happens If You Don’t Act Fast
Delaying treatment is dangerous. If you stop the drug within 24 hours of noticing symptoms, your risk of death drops from 15% to 5%. Wait too long, and the liver can’t recover. Kidneys may need dialysis. The immune system stays activated for months. Some patients need months of steroid treatment-starting with 1 mg/kg of prednisone daily, then slowly tapering over 4 to 8 weeks.
And you can’t just go home after the rash fades. You need close monitoring. Daily liver tests. Weekly blood counts. Infection screening. About 10% of DRESS patients develop bloodstream infections-E. coli, MRSA, Candida. Their skin is broken. Their immune system is exhausted. Hospitals treat them like transplant patients: strict isolation, IV antibiotics, antifungals.
There’s new hope. A 2022 study showed that adding anakinra-an IL-1 blocker used for rheumatoid arthritis-to steroids cut hospital stays from 18.5 days to 11.2 days. Tocilizumab, another immune drug, is being tested for steroid-resistant cases. These aren’t cures, but they’re steps forward.
Recovery and Long-Term Risks
Most people recover-if they’re caught early. But recovery isn’t the end. One in four survivors has lasting kidney damage. One in five needs ongoing specialist care. Autoimmune diseases can appear months later. Thyroid problems. Diabetes. Lupus. That’s why follow-up isn’t optional. It’s essential.
Patients who survived DRESS report the same thing: they wish they’d known sooner. They wish their doctor had asked about their meds. They wish they’d been told to stop the drug immediately. One woman on a patient forum wrote: “I lost three months of my life. My liver took a year to heal. But I’m alive because my dermatologist recognized the pattern.”
If you’ve been on allopurinol, carbamazepine, or Bactrim and now have a fever and rash, don’t wait. Don’t assume it’s a virus. Go to the ER. Ask: Could this be DRESS? Bring your medication list. Push for blood work-especially eosinophils and liver enzymes. Early action isn’t just helpful. It’s the difference between life and death.
What You Can Do Now
- If you’re taking allopurinol and have kidney disease, ask about HLA-B*58:01 testing.
- If you’re on carbamazepine or lamotrigine and develop a rash with fever, stop the drug and go to the hospital immediately.
- Keep a list of all medications you’ve taken in the last 8 weeks. Bring it to every doctor visit.
- If you’ve had DRESS before, never take the same drug again-or anything in the same class. Cross-reactivity is common.
- After recovery, schedule follow-ups with a nephrologist and endocrinologist. Autoimmune issues don’t always show up right away.
DRESS is rare. But it’s real. And it’s deadly. The good news? You can prevent it. You can survive it. But only if you know what to look for-and act before it’s too late.





Comments (12)
Glendon Cone
1 Jan 2026
Just had a friend go through this last year after starting allopurinol. Thought it was just a bad sunburn at first. Then she started coughing up phlegm and her eyes swelled shut. ER docs kept saying "virus." Took 3 weeks. She’s lucky to be alive. 🤢
Shae Chapman
2 Jan 2026
OMG I CRIED READING THIS. My cousin died from this and no one even suspected the meds. They just kept giving her more antibiotics. Like… why? 😭
Nadia Spira
3 Jan 2026
Let’s be real-this is just the medical-industrial complex’s way of monetizing idiocy. You don’t need a 2000-word essay to say "stop the drug if you break out." The fact that this is even a thing means doctors are still practicing witchcraft with lab reports. Eosinophils? Please. It’s called "pay attention to your patient."
henry mateo
4 Jan 2026
i read this and i just wanted to cry. my mom had this after taking sulfamethoxazole. they thought it was a viral rash. she ended up in icu for 17 days. her liver was at 1400. i wish i knew then what i know now. i keep her med list on my phone now. always.
Kunal Karakoti
5 Jan 2026
It's fascinating how the immune system, once activated by a foreign molecule, can spiral into self-destruction. The reactivation of HHV-6 as a secondary amplifier suggests a deeper interplay between virology and autoimmunity than we currently understand. Perhaps DRESS is not merely a drug reaction, but a window into the fragility of immune tolerance.
Kelly Gerrard
6 Jan 2026
This is why we need mandatory pharmacogenomic screening before prescribing high-risk meds. No excuses. Stop guessing. Test people. Save lives. Period
Henry Ward
7 Jan 2026
People keep acting like this is some new mystery. Nah. It’s just lazy medicine. If you don’t know the difference between a drug rash and DRESS, you shouldn’t be prescribing. And don’t get me started on how many patients get discharged too early. You think a rash fading means you’re fine? Nope. You’re just waiting for your liver to implode.
Aayush Khandelwal
9 Jan 2026
Man, this is like watching your body throw a mutiny. Allopurinol? More like "allopurinol: the silent saboteur." And HHV-6? The ghost in the machine that wakes up just to make things worse. We’re not just treating a rash-we’re negotiating with a rogue immune army. Wild stuff.
Sandeep Mishra
9 Jan 2026
Hey everyone-just wanted to say thank you to the OP for writing this. I’m a nurse in Mumbai and we see this more than you think, especially with gout patients on allopurinol. We don’t always have the labs or the time, but I always ask: "What meds did you start in the last month?" That one question has saved two lives this year. Keep sharing this. 🙏
Joseph Corry
10 Jan 2026
Oh, so now we’re giving out life-saving advice like it’s a TED Talk? How quaint. Let me guess-the next post will be titled "How to Avoid Death by Ibuprofen: A Step-by-Step Guide for the Clinically Unaware." Meanwhile, real medicine is happening in ICUs, not in Reddit threads full of emotional anecdotes.
Colin L
11 Jan 2026
I’ve been thinking about this for days. You know what’s really terrifying? That this isn’t about drugs at all-it’s about the collapse of the doctor-patient relationship. We’ve outsourced diagnosis to algorithms and checklists, and now we’re surprised when the human body doesn’t fit neatly into a box labeled "viral exanthem." The real tragedy isn’t DRESS-it’s that we’ve forgotten how to listen. And when you stop listening, the body screams louder. And louder. And then it just… stops.
Hayley Ash
11 Jan 2026
Wow so much drama over a rash lmao maybe people should stop taking meds they dont need