Estrogen and Warfarin Interaction: What You Need to Know
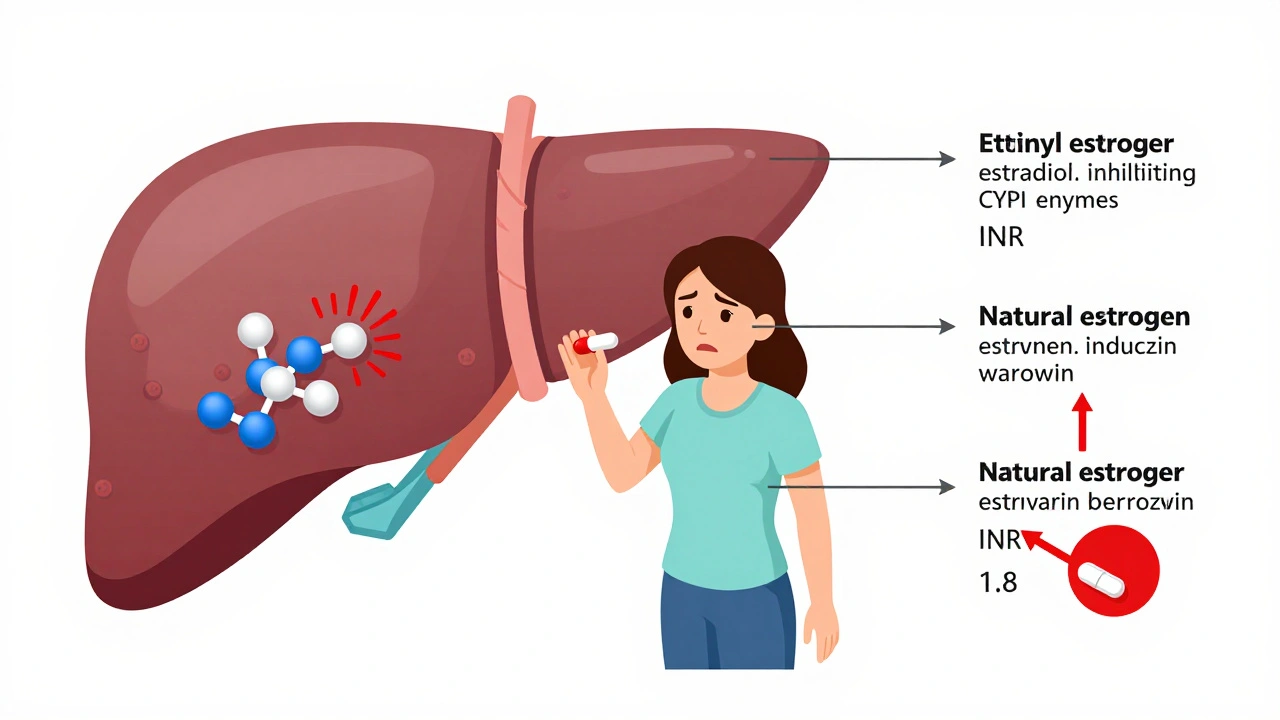
When you take estrogen, a hormone used in birth control or hormone replacement therapy. Also known as oral contraceptives or HRT, it can change how your body handles blood thinners like warfarin. Many people don’t realize that estrogen doesn’t just affect your cycle or hot flashes—it can make warfarin stronger, increasing your risk of bleeding. This isn’t a rare edge case. It’s a well-documented interaction that shows up in hospital records and pharmacy alerts across North America.
Warfarin, a vitamin K antagonist used to prevent dangerous clots in people with atrial fibrillation, deep vein thrombosis, or mechanical heart valves. Also known as Coumadin, it’s one of the most commonly prescribed anticoagulants in Canada and the U.S. But its narrow safety window means even small changes in your body can push it into dangerous territory. Estrogen raises levels of clotting factors like Factor VII and IX, which warfarin tries to suppress. When you start or stop estrogen, your INR can swing up or down—sometimes within days. That’s why people on both meds need frequent blood tests. One study from the Canadian Journal of Cardiology found that over 30% of women on estrogen therapy saw their INR rise above the target range within the first two weeks.
This isn’t just about pills. If you’re switching from a patch to a pill, changing brands, or even starting a new OTC supplement like black cohosh, your body’s response to warfarin can shift. Estrogen isn’t the only player—vitamin K intake, liver function, and even gut bacteria play roles. But estrogen is one of the top five triggers for warfarin instability, according to the FDA’s adverse event database. You don’t need to quit your hormone therapy. But you do need to know the signs: unusual bruising, nosebleeds that won’t stop, dark stools, or sudden joint pain. These aren’t just side effects—they could be early warnings of internal bleeding.
What you’ll find in the posts below are real-world guides from people who’ve been through this. From how to talk to your pharmacist about timing your doses, to what to do if your INR spikes after starting birth control, to how to track changes without panic. These aren’t theory pages. They’re practical, tested advice from patients and clinicians who’ve seen the fallout—and the fixes.
Estrogen can raise or lower your INR when you're on warfarin, increasing bleeding or clotting risk. Learn how birth control, HRT, and your genes affect warfarin dosing and what steps to take to stay safe.