Estrogen Interactions with Warfarin: What You Need to Know About Bleeding Risk and Dose Changes
Warfarin Estrogen Interaction Calculator
Estimate Your Warfarin Dose Adjustment
Based on evidence from clinical studies and guidelines, this calculator helps determine the appropriate warfarin dose adjustment when starting or stopping estrogen-containing products.
When you're on warfarin, even small changes in your meds can throw your blood clotting off balance. One of the most common yet confusing interactions happens with estrogen - whether it's from birth control pills, hormone replacement therapy, or other estrogen-containing products. This isn't just a theoretical concern. Real patients have seen their INR jump from 2.5 to 4.3 within days of starting estrogen, leading to dangerous bleeding risks. Others saw their INR drop, making their blood clot more easily. The truth? Estrogen and warfarin don't play nice together - and the way they interact depends on which estrogen you're taking, your genes, and even what else you're on.
How Estrogen Changes Warfarin’s Effect
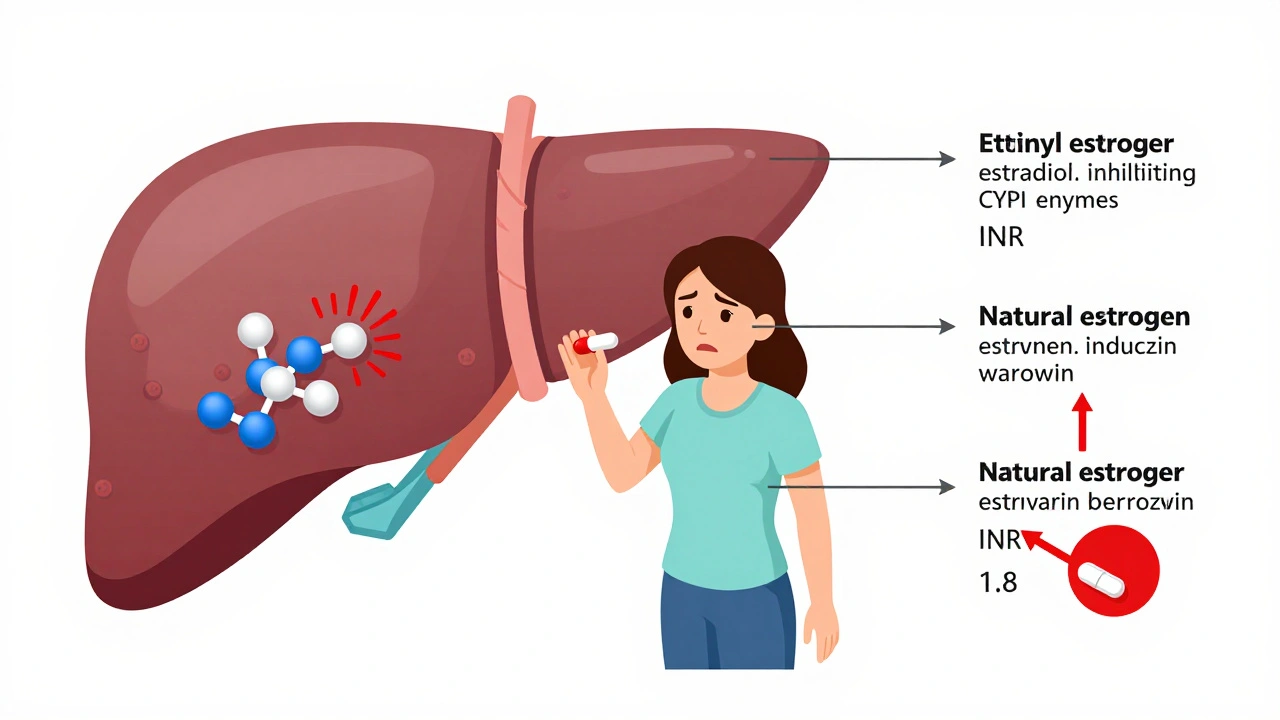
Warfarin doesn’t work the same way in everyone. It’s broken down in the liver by enzymes called CYP450s - mainly CYP2C9, CYP1A2, and CYP3A4. Estrogen compounds can either speed up or slow down these enzymes, which means warfarin can either build up in your body or get cleared too fast.
Natural estrogen, like estradiol, tends to induce certain liver enzymes. That means your body starts breaking down warfarin faster. Your INR might drop. You’re at higher risk for clots - maybe a DVT or stroke - without even knowing it.
But synthetic estrogen, like ethinyl estradiol in birth control pills, does the opposite. It inhibits CYP1A2 and CYP2C19. That slows down warfarin metabolism. Warfarin builds up. Your INR climbs. Now you’re at risk for bleeding - nosebleeds, bruising, or worse, internal bleeding.
This isn’t just guesswork. A 2009 case study in The Annals of Pharmacotherapy tracked a 28-year-old woman whose INR jumped from 2.4 to 4.3 after starting a birth control pill. Her warfarin dose had to be cut from 5 mg to 3.5 mg. That’s a 30% reduction - all because of one new pill.
Why Some People Are More at Risk
Not everyone reacts the same way. Your genes matter. About 30% of people have a variant in the CYP2C9 gene - called *2 or *3 - that makes them break down warfarin much slower. If you’re one of them, even a small dose of estrogen can push your INR into dangerous territory.
Then there’s VKORC1. If you carry the -1639G>A variant, your body is extra sensitive to warfarin. You need less of it to get the same effect. Add estrogen on top of that, and you’re playing with fire. Studies show these patients need 30-50% lower warfarin doses just to stay in range - and estrogen can make that balance even trickier.
Women between 18 and 45 are especially vulnerable. The INR Registry analyzed over 15,000 patients and found those on estrogen-containing contraceptives had 1.8 times higher risk of INR above 4.0 - the level where bleeding risk spikes. That’s not a small number. It’s a red flag.
How This Compares to Other Drug Interactions
Warfarin has dozens of drug interactions. Antibiotics like ciprofloxacin or trimethoprim-sulfamethoxazole can spike INR by 2.5 to 3 times. SSRIs like fluoxetine double bleeding risk. Amiodarone? It can force you to cut your warfarin dose by 40%.
Estrogen interactions are different. They usually cause smaller INR shifts - often between 0.5 and 1.5 points. But here’s the catch: even a 0.5-point rise in INR can increase bleeding risk by 20-30%. That’s why experts say you can’t ignore them.
Compare that to antibiotics: they hit hard and fast. Estrogen? It’s sneaky. It might take a few days to show up on your INR test. That delay is why so many patients get caught off guard.

What Happens When You Start or Stop Estrogen
Timing matters. If you start estrogen - whether it’s birth control, HRT, or a patch - your INR might not change right away. It can take 3 to 7 days for the enzyme effects to kick in. That’s why guidelines say: check your INR within 3 to 5 days after starting estrogen.
And don’t forget stopping. If you quit estrogen - say, you’re switching birth control or ending HRT - your body suddenly loses the enzyme inhibition or induction. Warfarin metabolism flips back. Your INR can swing the other way. One patient on Reddit said her INR dropped from 3.0 to 2.0 after stopping HRT. Her doctor had to increase her warfarin dose by 15% to keep her protected.
That’s why monitoring doesn’t stop after the first test. Check again at 7 to 14 days. And if you’re on long-term estrogen, keep checking every 2 to 4 weeks until things stabilize.
What Doctors Do About It
Most anticoagulation clinics have a playbook. If you’re starting estrogen and your INR rises, they’ll typically reduce your warfarin dose by 10-25%. If your INR drops, they’ll increase it by 10-20%. It’s not one-size-fits-all. It’s based on your baseline INR, your age, your weight, and your genetic profile.
Some clinics now use pharmacogenetic testing. The International Warfarin Pharmacogenetics Consortium (IWPC) developed a dosing algorithm that combines your CYP2C9 and VKORC1 genes with age, weight, and other meds. It’s been tested on over 5,000 people and improves dose accuracy by 30-35%. That means fewer dangerous INR swings - and fewer hospital visits.
Electronic INR Monitoring Systems (EIMS) are also helping. In 47 U.S. clinics, these digital tools flag potential estrogen-warfarin interactions before they become problems. One study showed they cut interaction-related bleeding events by 32%.
What You Should Do
If you’re on warfarin and considering estrogen - or already taking it - here’s what you need to do:
- Don’t start or stop estrogen without telling your anticoagulation provider.
- Get your INR checked within 3-5 days after starting or stopping estrogen.
- Check again at 7-14 days, even if the first result looks fine.
- Keep a log of your doses, INR results, and any new meds or supplements.
- Ask if you’re a candidate for genetic testing - especially if you’ve had unstable INRs before.
And if you’re on birth control? Talk to your doctor about alternatives. Progestin-only pills, IUDs, or implants don’t carry the same interaction risk. For women over 50 on HRT, consider non-estrogen options like selective estrogen receptor modulators (SERMs) if appropriate.

Why Warfarin Is Still Used - Even With DOACs Around
You’ve probably heard about direct oral anticoagulants (DOACs) like apixaban or rivaroxaban. They don’t need INR checks. They have fewer interactions. And yes, they’ve taken over 68% of the oral anticoagulant market since 2013.
But warfarin hasn’t disappeared. It’s still the only option for people with mechanical heart valves. It’s preferred for those with antiphospholipid syndrome. And for some, it’s cheaper. The American College of Cardiology estimates 1.8 million Americans will still need warfarin through 2030.
That means understanding estrogen interactions isn’t just academic. It’s life-saving.
Common Myths About Estrogen and Warfarin
Myth: All estrogen affects warfarin the same way.
Truth: Natural estradiol and synthetic ethinyl estradiol do the opposite things. One lowers INR. The other raises it.
Myth: If my INR is stable, I don’t need to worry about estrogen.
Truth: Estrogen can shift your INR weeks after you start it. Stability now doesn’t mean stability later.
Myth: Only birth control pills matter.
Truth: Patches, gels, rings, and HRT all contain estrogen. All of them can interact.
Myth: My doctor would have told me if this was a problem.
Truth: A 2021 survey found that 57% of pharmacists found it hard to tell if an INR change was due to estrogen or something else - like diet, illness, or another drug. You have to speak up.
Can I take birth control if I’m on warfarin?
Yes - but not without caution. Estrogen-containing birth control can raise your INR and increase bleeding risk. Your doctor will likely check your INR before you start, then again at 3-5 days and 7-14 days after. Many patients switch to progestin-only pills, IUDs, or implants, which don’t interact with warfarin. Always talk to your anticoagulation team before starting any hormonal contraceptive.
How long after starting estrogen should I check my INR?
Check your INR within 3 to 5 days of starting estrogen. Changes in liver enzyme activity can take a few days to affect warfarin levels. A second check at 7-14 days is recommended to confirm stability. Don’t wait for symptoms - bleeding or clotting can happen without warning.
Does hormone replacement therapy (HRT) affect warfarin?
Yes. Estrogen in HRT - whether pills, patches, or gels - can either raise or lower your INR depending on the type and dose. Most often, it increases INR, raising bleeding risk. Patients on HRT should have INR checks at 3-5 days and again at 1-2 weeks after starting or changing their HRT. Dose adjustments of 10-25% are common.
Why does my INR go up and down even when I take the same dose?
Many things can cause INR swings - diet (especially vitamin K), illness, alcohol, other meds, and yes - estrogen. If you’re on estrogen, even small changes in your regimen can shift your INR. That’s why consistent monitoring is critical. Keep a log of everything you take, eat, or feel. Bring it to every appointment. Your care team needs that data to make sense of the numbers.
Should I get genetic testing for warfarin sensitivity?
If you’ve had unstable INRs, frequent dose changes, or bleeding/clotting events on warfarin, yes. Testing for CYP2C9 and VKORC1 variants can help predict your ideal dose and reduce interaction risks. It’s especially helpful if you’re also on estrogen. The FDA updated warfarin labeling in 2023 to support genetic testing. Many clinics now offer it as part of routine care.
Final Takeaway
Estrogen doesn’t have to be off-limits if you’re on warfarin - but it demands attention. It’s not a simple yes or no. It’s a conversation with your care team, a plan for monitoring, and a willingness to track your INR closely. The interaction is real, predictable, and manageable. Ignore it, and you’re gambling with your health. Stay informed, stay vigilant, and don’t assume your doctor will catch every change. You’re your own best advocate.






Comments (17)
Nikhil Pattni
9 Dec 2025
Yo, this is wild - I’ve been on warfarin for AFib since 2020 and started estradiol gel last year for perimenopause. My INR went from 2.8 to 4.1 in 4 days. Doc didn’t even mention estrogen as a possible culprit until I brought up the patch I was using. Turns out, natural estrogen can *induce* enzymes? I thought all estrogen was the same. Now I’m on a 20% lower dose and checking INR every 5 days. Pro tip: keep a log. I use Google Sheets. It’s nerdy but saves lives. 📊
Arun Kumar Raut
11 Dec 2025
Hey, I get that this is super technical, but if you're on warfarin and thinking about any kind of hormone stuff, just talk to your pharmacist. They’re the real MVPs. I used to think doctors knew everything, but my pharmacist caught my INR spike before my doctor even saw it. She said, 'You started that new patch, right?' Like, how did she know? She just pays attention. You don’t need to be a scientist - just be honest and ask questions. 💪
precious amzy
11 Dec 2025
One cannot help but observe the profound epistemological rupture between clinical dogma and patient agency in this discourse. The very notion that 'estrogen' is a monolithic entity is a reductive anthropocentric fallacy - a linguistic artifact of pharmaceutical capitalism. One must interrogate the ontological status of 'ethinyl estradiol' as a synthetic imposition upon natural hormonal flux. Is it not the body's own homeostasis that is pathologized? The INR, a mere metric, becomes a proxy for control - a Foucauldian biopower enacted through lab reports and dose adjustments. The real crisis is not pharmacokinetics - it is the surrender of bodily sovereignty to algorithmic medicine.
William Umstattd
12 Dec 2025
Let me be crystal clear: if you’re taking estrogen while on warfarin and you haven’t had a pharmacogenetic test, you’re playing Russian roulette with your internal organs. This isn’t 'maybe' - it’s a documented, predictable, and preventable disaster. The FDA updated the labeling in 2023. Your doctor should be offering this test. If they’re not, get a new doctor. I’ve seen three patients bleed out because their 'stable' INR suddenly crashed - all because someone assumed 'it’s just birth control.' It’s not. It’s a chemical grenade in your liver. Stop being casual about this.
Andrea Beilstein
13 Dec 2025
So many people treat warfarin like it’s aspirin. It’s not. It’s a precision instrument. And estrogen? It’s not just a pill. It’s a signal. Your liver hears it. Your enzymes hear it. Your clotting cascade hears it. You can’t just 'take it' and hope for the best. I’m a nurse and I’ve watched people get strokes because they thought 'I’m young, I’m fine.' You’re not fine. You’re a walking lab experiment. And if you’re on a patch or gel - yes, it still counts. Skin doesn’t make it safe. It makes it sneakier.
Brianna Black
15 Dec 2025
As a woman who’s been on warfarin for 12 years and HRT for 7, I can tell you - this is the most important thing no one tells you. The first time I stopped HRT to 'detox,' my INR dropped from 2.9 to 1.8 in two weeks. I didn’t feel anything. No clots, no symptoms. Just a number on a screen that could’ve killed me. My anticoagulation clinic had me increase my dose by 18%. I cried. I felt so stupid. But I learned. Now I track everything. Even my coffee intake. Because your body doesn’t care what you 'think' you’re doing. It just reacts. And it doesn’t apologize.
Stacy Tolbert
15 Dec 2025
I just want to say - I’m so tired of people acting like this is just 'medical jargon.' This is my life. I had a brain bleed at 34 because my INR spiked after starting birth control. I’m fine now, but I have seizures. I have to take meds. I can’t drive. I can’t have kids. And the worst part? No one warned me. My OB said 'it’s fine.' My cardiologist said 'it’s rare.' It’s not rare. It’s just not talked about. If you’re on warfarin and thinking about estrogen - stop. Talk to someone who’s been there. Don’t trust a Google search. I wish I had.
Ryan Brady
16 Dec 2025
Why are we even talking about this? Just switch to the new blood thinners. They don’t need all this BS. Why are we still using warfarin in 2025? It’s 2025. We have apps that track your INR. We have AI that predicts interactions. But no - we’re still making women count their vitamin K and check their blood every week because 'it’s cheaper.' I get it - insurance sucks. But this is America. We have the tech. We just don’t care. 😒
Raja Herbal
17 Dec 2025
So you’re telling me the same estrogen that gives me glowing skin also makes my blood turn to jelly? Cool. So I guess I’m paying for beauty with a chance of bleeding out. Thanks, patriarchy. 🙃
Iris Carmen
19 Dec 2025
wait so if i use the estrogen patch… does it count? like i thought only pills mattered? 🤔
Rich Paul
20 Dec 2025
bro i got my INR checked after i started my estrogen gels and it was fine so i just stopped checking. cmon man, i got a job, i got kids, i don’t have time for this. my doc said 'if you feel weird, come back' - and i haven’t felt weird. so… i’m good? 🤷♂️
Noah Raines
21 Dec 2025
Just got my genetic test back - CYP2C9*3 and VKORC1 -1639AA. Doc said I’m a 'super responder.' My baseline dose is 1.5mg. I started estradiol gel and my INR jumped to 4.6. They cut me to 1mg. Now I’m stable. I’m not a lab rat. I’m just a guy who got lucky. If you’re on warfarin and you’ve ever had a weird INR swing - get tested. It’s not expensive. It’s not scary. It’s just smart. 💡
Katherine Rodgers
21 Dec 2025
Oh wow. So the 'natural' estrogen is the one that makes your INR drop? So the 'synthetic' one is the dangerous one? That’s ironic. Because the 'natural' one is what Big Pharma sells as 'bio-identical' and charges $200 a month for. Meanwhile, the cheap generic birth control pill? The one that actually spikes INR? That’s the one your insurance covers. So we’re paying extra for a 'safer' option that’s actually worse? Classic. 🤡
Lauren Dare
21 Dec 2025
Can we pause for a second and acknowledge that this entire conversation is framed around women’s bodies being medicalized? The fact that we have to worry about 'estrogen interactions' at all implies that hormonal regulation is a problem - not a normal function. Why is warfarin the baseline? Why not design anticoagulants that don’t interfere with endogenous physiology? The real issue isn’t estrogen. It’s that we’re using a 70-year-old drug on a 21st-century population with complex endocrine needs. The science is outdated. The system is broken. The burden is on the patient. Again.
Christian Landry
22 Dec 2025
my cousin’s on warfarin and started the patch for menopause - she didn’t check her INR for 3 weeks. ended up in the ER with a GI bleed. they said it was 'classic estrogen interaction.' she’s fine now but says she’ll never trust her doctor again. i told her: next time, check the INR before you even start the patch. just do it. it takes 5 minutes. 🙏
Katie Harrison
22 Dec 2025
Thank you for this. I’ve been on warfarin since 2018. Started HRT last year. I had no idea that gels and patches mattered. I thought only pills did. I’ve been checking my INR religiously since - every 7 days for the first month, now every 3 weeks. I’m stable. But I’m terrified to change anything. I’ve started keeping a journal. I write down everything: food, sleep, stress, meds. It’s obsessive. But I’d rather be obsessive than dead. 🌿
Mona Schmidt
23 Dec 2025
Just want to add - if you’re on warfarin and you’re considering estrogen, don’t just ask your doctor. Ask your pharmacist. They’re trained in drug interactions. They see this every day. My pharmacist caught that my new estrogen cream was interacting with my warfarin before my doctor even saw the INR result. She called me at 7 p.m. on a Friday. I cried. She didn’t have to do that. But she did. That’s the kind of care we need more of. Not just algorithms. Real people. 💛