Fluoroquinolone Resistance: What It Is, Why It Matters, and What You Can Do
When fluoroquinolone resistance, the ability of bacteria to survive and multiply despite treatment with fluoroquinolone antibiotics like ciprofloxacin or levofloxacin. Also known as quinolone resistance, it’s one of the fastest-growing threats in modern medicine. These drugs used to be go-to treatments for urinary infections, pneumonia, and even anthrax—but now, in many places, they don’t work like they used to. The problem isn’t just that bacteria are getting stronger. It’s that we’ve overused these antibiotics in ways that made resistance inevitable.
Antibiotic resistance, the broader phenomenon where bacteria evolve to survive drugs meant to kill them isn’t new, but fluoroquinolone resistance is especially concerning because these antibiotics are broad-spectrum—they hit a wide range of bacteria. That means when they stop working, doctors lose a major tool. Bacterial resistance, the specific mechanism by which bacteria develop defenses like enzyme production or efflux pumps to neutralize or eject antibiotics happens fast when these drugs are used too often or for the wrong reasons—like treating viral colds or using them in livestock to speed up growth. The result? More people get sick longer, end up in the hospital, or even die from infections that were once easy to fix.
What’s worse, fluoroquinolone resistance doesn’t happen in a vacuum. It’s tied to other problems we see in the posts below—like antibiotic side effects, serious reactions like tendon ruptures, nerve damage, and long-term fatigue that can follow even short courses of these drugs. People stop taking them early because of side effects, which only feeds resistance. Or they take them without a prescription, thinking they’ll help with a sore throat—when they won’t. And when resistance builds, doctors are forced to use stronger, more toxic, or more expensive alternatives. That’s why understanding fluoroquinolone resistance isn’t just for doctors—it’s for anyone who’s ever taken an antibiotic.
You’ll find real-world examples in the posts below: comparisons of antibiotics like Zyvox and Secnidazole, discussions on how misuse fuels resistance, and guides on when to avoid certain drugs altogether. No fluff. No marketing. Just clear, practical info on how to protect yourself and others from the growing danger of drugs that no longer work. This isn’t about fear. It’s about knowing when to say no—and when to ask for something better.
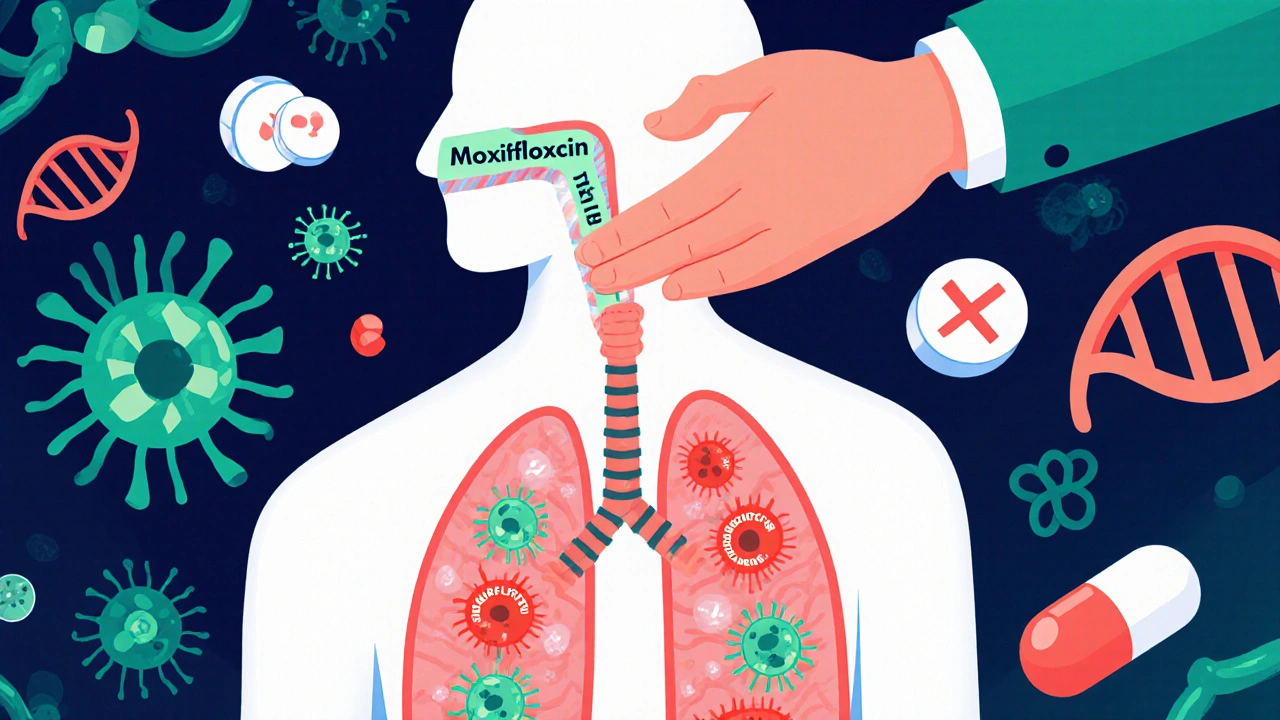
Moxifloxacin resistance is rising due to overuse and incomplete courses. Learn the real causes, how to prevent it, and what doctors and patients can do to protect this vital antibiotic.