Glioblastoma: Causes, Treatments, and What You Need to Know
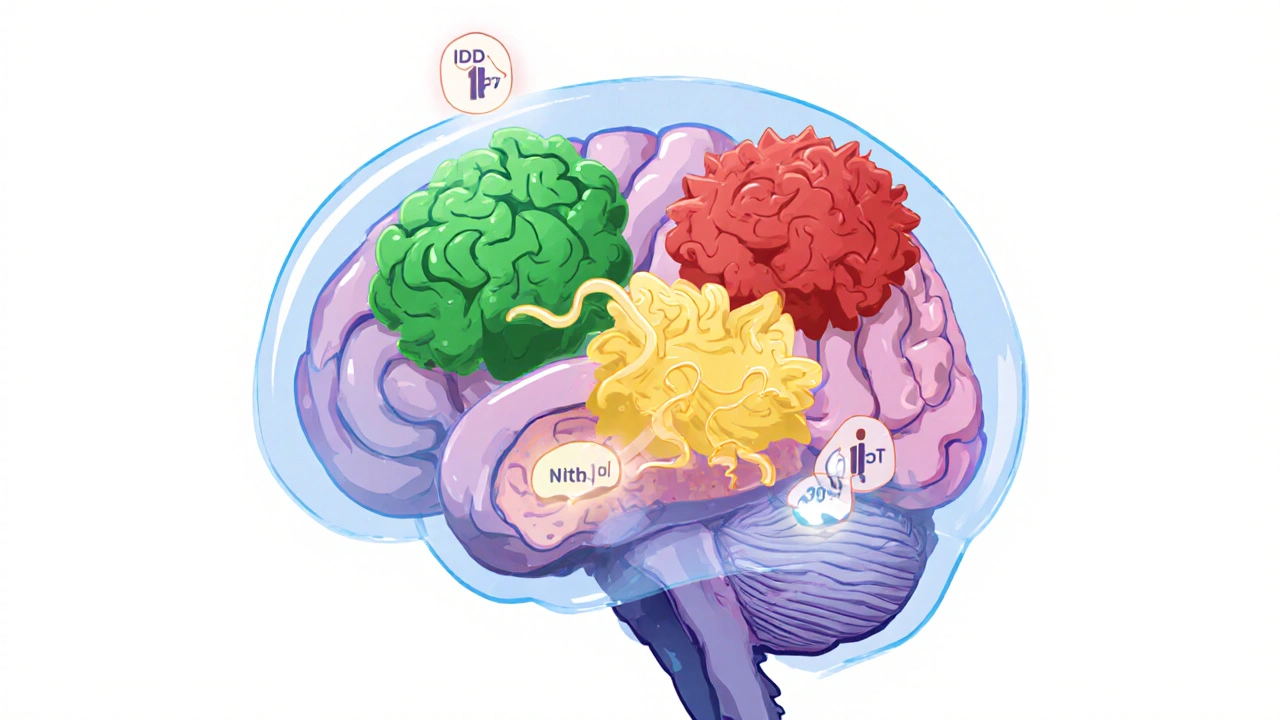
When someone is diagnosed with glioblastoma, a fast-growing, malignant brain tumor that starts in glial cells. Also known as GBM, it's the most common and aggressive type of primary brain cancer in adults. Unlike slower-growing tumors, glioblastoma spreads quickly through brain tissue, making complete removal nearly impossible. It doesn’t usually spread to other parts of the body, but within the brain, it’s relentless.
Most cases have no clear cause, though a small number are linked to rare genetic syndromes like Li-Fraumeni or neurofibromatosis. Exposure to high-dose radiation is the only proven environmental risk. Age matters too—over 65 is when most cases appear. Men are slightly more likely to get it than women. There’s no proven link to cell phones, power lines, or diet, despite what you might hear online.
Standard treatment starts with surgery to remove as much of the tumor as safely possible. But because glioblastoma tendrils grow into healthy brain tissue, surgeons can’t get it all. That’s why radiation and chemotherapy follow, usually with temozolomide. Even with this combo, recurrence is common. Newer approaches like tumor-treating fields (TTFields), which use electric fields to disrupt cancer cell division, have shown modest survival improvements in clinical trials. Immunotherapy and targeted drugs are being tested, but so far, none have broken through as a game-changer.
The survival rate, the percentage of people alive a certain time after diagnosis is sobering. About 5% of patients live five years or longer. Median survival is around 15 months with treatment. Without it, survival drops to just a few months. These numbers aren’t just statistics—they reflect real people facing tough choices every day.
What’s changing? Research is focusing on personalized medicine. Scientists are analyzing tumor genetics to find mutations that might respond to specific drugs. CAR-T cell therapy, which reprograms a patient’s own immune cells to attack cancer, is being tested in early trials. Liquid biopsies that detect tumor DNA in blood could soon help track how the cancer evolves without repeated brain surgeries.
There’s no cure yet. But the landscape is shifting. What used to be a single treatment path is now a patchwork of options—some proven, some experimental. Patients aren’t just waiting for the next step; they’re part of a larger effort to find better ones. The posts below cover everything from how chemotherapy affects glioblastoma patients, to the latest on radiation techniques, to what real people experience when managing symptoms and side effects. You won’t find fluff here—just straight talk on what works, what doesn’t, and what’s on the horizon.
Understand brain tumor types, WHO CNS5 grading, and modern treatments including vorasidenib and molecular diagnostics. Learn how IDH mutations and 1p/19q codeletion impact survival and therapy choices.