Hormonal Contraceptives and Blood Thinners: Risks, Interactions, and What You Need to Know
When you’re taking hormonal contraceptives, birth control pills, patches, or IUDs that contain estrogen or progestin to prevent pregnancy. Also known as oral contraceptives, they work by controlling hormone levels—but that same mechanism can affect how your body handles other drugs. Many people don’t realize these same hormones can increase the risk of blood clots, which directly clashes with the purpose of blood thinners, medications like warfarin, apixaban, or enoxaparin used to stop dangerous clots from forming. Also known as anticoagulants, they’re prescribed for conditions like atrial fibrillation, deep vein thrombosis, or after surgery. Mixing the two isn’t just a technical concern—it’s a real safety issue that can lead to life-threatening complications.
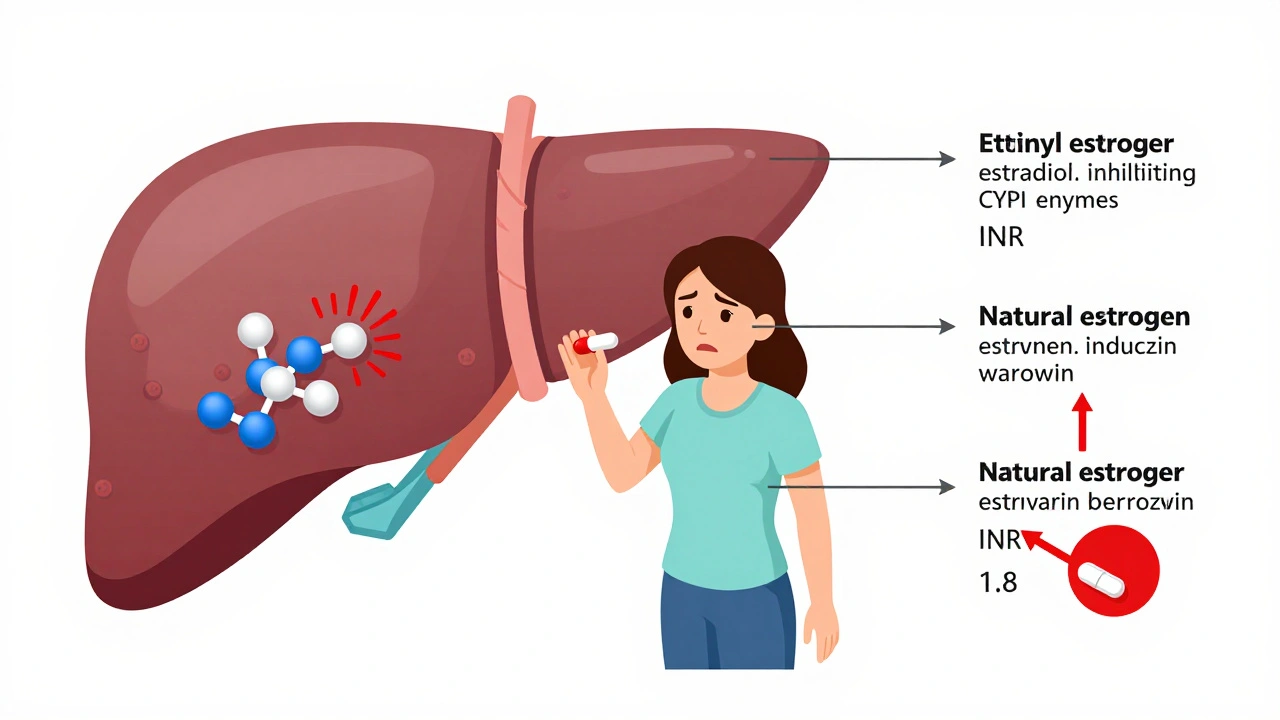
Estrogen in hormonal contraceptives boosts clotting factors in your blood. That’s why they’re effective at preventing pregnancy—but it also means they can undo the work of blood thinners. If you’re on a blood thinner for a history of clots or a heart condition, adding birth control can push your clotting risk into dangerous territory. On the flip side, some blood thinners can make hormonal contraceptives less effective, increasing the chance of unintended pregnancy. This isn’t theoretical: studies show women on both types of drugs have a higher rate of venous thromboembolism, a condition where clots form in deep veins, often in the legs, and can travel to the lungs than those on either drug alone. And if you’re already at risk—due to obesity, smoking, age over 35, or a genetic clotting disorder—the danger multiplies.
It’s not just about skipping a pill. The real problem is that most people don’t connect these two meds in their head. You might be on warfarin after a pulmonary embolism, then get prescribed a new birth control pill without your doctor knowing your full history. Or your OB-GYN prescribes hormonal contraception without checking if you’re on an anticoagulant. That’s why medication reviews matter. If you’re taking five or more drugs—as mentioned in our guide on preparing for a medication review—you’re at higher risk for hidden interactions. Pharmacists see this all the time: patients who think their birth control is "just birth control" and don’t mention it during a blood thinner checkup.
There are safer paths. Progestin-only pills, implants, or IUDs don’t carry the same clotting risk as estrogen-based options. For some women, switching to a progestin-only method while staying on a blood thinner is the smartest move. Others might use non-hormonal birth control like copper IUDs or condoms. The key isn’t avoiding contraception—it’s choosing the right one for your health profile. And if you’re on a blood thinner like enoxaparin, monitoring your anti-Xa levels—as covered in our guide on anti-Xa testing—can help catch when the balance is off.
Below, you’ll find real-world guides on spotting drug reactions, understanding black box warnings, managing side effects, and avoiding dangerous combinations. These aren’t theoretical articles—they’re tools used by people who’ve been through this. Whether you’re on birth control, a blood thinner, or both, the information here will help you ask the right questions, spot red flags, and work with your care team to stay safe.
Estrogen can raise or lower your INR when you're on warfarin, increasing bleeding or clotting risk. Learn how birth control, HRT, and your genes affect warfarin dosing and what steps to take to stay safe.