Pharmaceutical Manufacturing: How Drugs Are Made and Why It Matters
When you pick up a pill or get an injection, you’re relying on pharmaceutical manufacturing, the complex process of producing medicines at scale with strict quality and safety standards. Also known as drug production, it’s the invisible engine behind every prescription, over-the-counter remedy, and life-saving injection you use. This isn’t just mixing chemicals in a lab—it’s a global system of precision engineering, regulatory oversight, and supply chain logistics that determines whether you get your medicine on time, at the right dose, and without harmful contaminants.
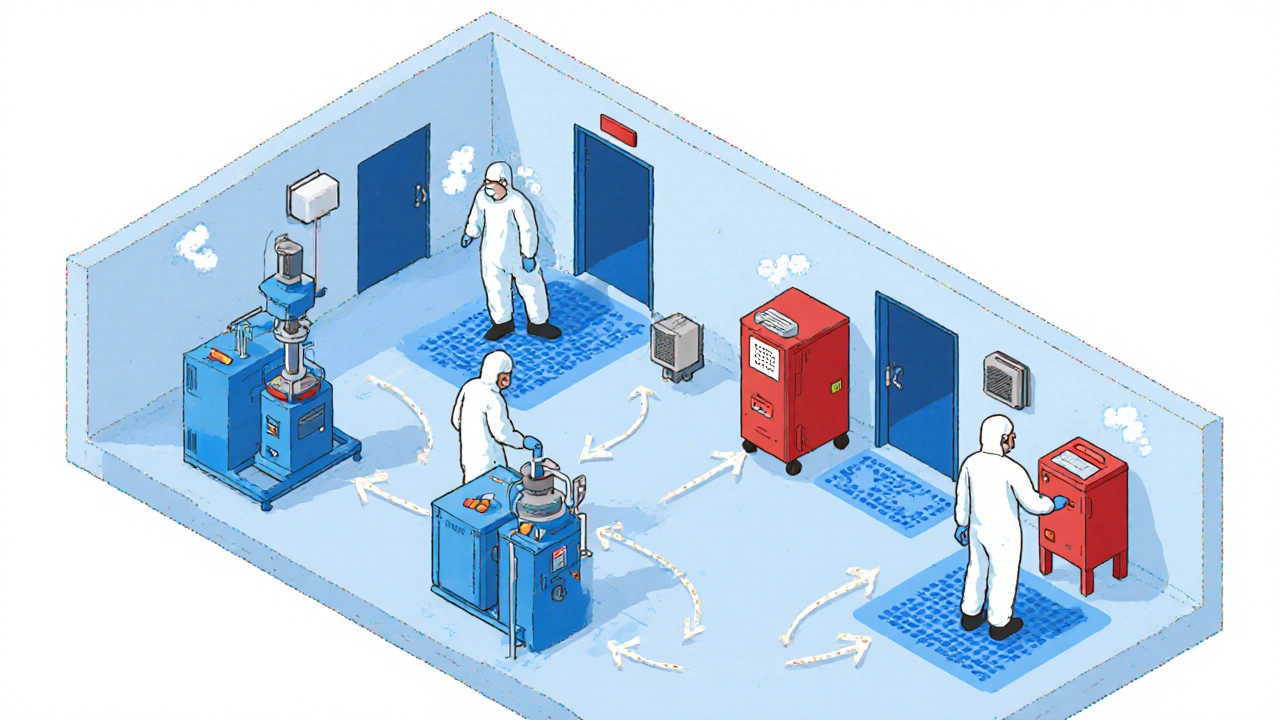
Behind every sterile injectable, a drug delivered directly into the bloodstream, requiring absolute cleanliness to prevent infection is a cleanroom environment where even a speck of dust can ruin a batch. That’s why hospital pharmacies are often the first to feel the impact when manufacturing fails—like the recent shortages of anesthetics and chemotherapy drugs. These aren’t random glitches. They’re symptoms of a system stretched thin by rising demand, geopolitical supply risks, and the rising cost of meeting FDA and Health Canada standards. Meanwhile, generic drugs, lower-cost versions of brand-name medications approved through strict equivalence testing make up over 90% of prescriptions in the U.S., but their production is often outsourced to countries with looser oversight, creating hidden vulnerabilities. The therapeutic equivalence, the official FDA rating that tells pharmacists which generics can safely replace brand drugs you see on your prescription label? That’s the result of years of testing, bioequivalence studies, and manufacturing audits—all tied directly to how the drug was made.
It’s not just about pills and injections. The way a drug is manufactured affects its side effects, its cost, and even its environmental footprint. Take cetirizine, a common allergy medication whose production generates chemical waste and uses large amounts of water. Newer facilities are switching to green chemistry to cut pollution, but many still rely on outdated methods. And when a company cuts corners on quality control, it’s not just a regulatory issue—it’s a patient safety issue. That’s why monitoring anti-Xa levels, a blood test used to track the effectiveness of blood thinners like enoxaparin matters so much: if the drug’s concentration is off due to inconsistent manufacturing, the risk of clots or bleeding skyrockets.
What you’ll find below is a collection of real stories from the front lines of this system—how drug shortages hit hospitals, why some generics work better than others, how antibiotic resistance ties back to production practices, and what happens when a life-saving injection runs out. These aren’t abstract policy debates. They’re daily realities for patients, pharmacists, and doctors. Whether you’re trying to lower your copay, avoid dangerous interactions, or just understand why your medicine isn’t available, the answers start here—with how drugs are made.
Contamination controls in generic drug manufacturing prevent dangerous adulteration through strict cleaning protocols, cleanroom design, and real-time monitoring. Learn how facilities stay compliant and avoid costly recalls.