Preventing Antibiotic Resistance: What You Need to Know
When you take an antibiotic, a medicine designed to kill or slow down harmful bacteria. Also known as antibacterial drugs, they save lives—but only when used correctly. Misuse turns them into a ticking time bomb for everyone. Every time you take an antibiotic when you don’t need it, or don’t finish the full course, you help create superbugs, bacteria that no longer respond to common antibiotics. These aren’t science fiction. They’re in hospitals, gyms, and homes right now.
Antibiotic resistance doesn’t just happen because doctors prescribe too much. It’s also because people expect antibiotics for every cold, cough, or sore throat—even when it’s a virus. Viruses don’t respond to antibiotics. Taking them anyway doesn’t speed up recovery. It just gives bacteria a chance to adapt. Antibiotic stewardship, the practice of using antibiotics only when necessary and in the right way is the only real defense. It’s not just for doctors. It’s for you too.
Some people stop taking antibiotics as soon as they feel better. That’s a mistake. Even if symptoms vanish, some bacteria may still be alive. These survivors are often the toughest ones—and they pass on their resistance to future generations. Others save leftover pills for later, or share them with family. That’s dangerous. Every antibiotic is prescribed for a specific infection, weight, and duration. Using the wrong one can make things worse.
Antibiotics aren’t harmless. They can cause antibiotic side effects, ranging from stomach upset to life-threatening allergic reactions. They also wipe out good bacteria in your gut, which can lead to long-term digestive issues. That’s why it’s critical to only use them when there’s a confirmed bacterial infection. Not every fever needs an antibiotic. Not every earache does either.
What you can do? Ask your doctor: "Is this really a bacterial infection?" and "What happens if I don’t take this?" If they say it’s viral, don’t push. If they say you need it, take every pill. Don’t skip doses. Don’t save them. And never use someone else’s prescription. Simple habits like washing your hands, staying up to date on vaccines, and avoiding unnecessary antibiotics are the best tools we have to stop superbugs from spreading.
Below, you’ll find real guides that break down exactly how antibiotics are misused, what alternatives exist, how to recognize when they’re needed, and how to protect yourself and your family. These aren’t theory pieces. They’re practical, real-world advice from people who’ve seen the damage firsthand—and know how to fix it.
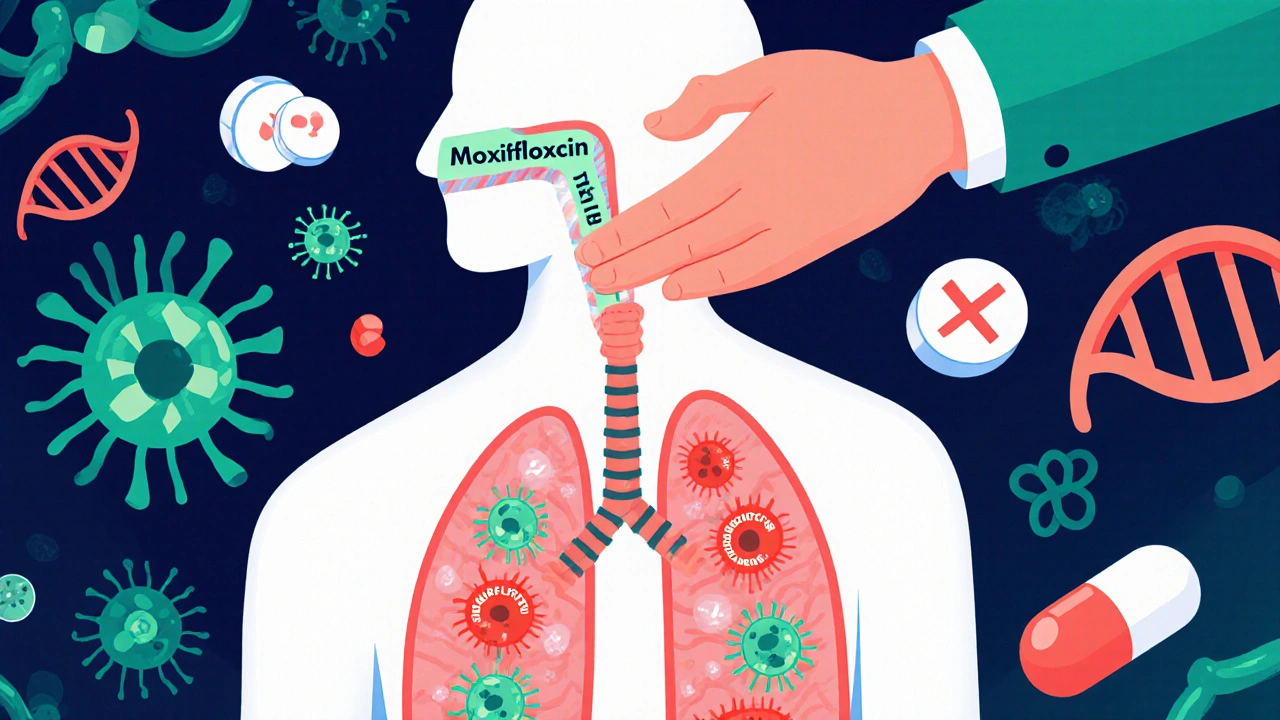
Moxifloxacin resistance is rising due to overuse and incomplete courses. Learn the real causes, how to prevent it, and what doctors and patients can do to protect this vital antibiotic.