Therapy for Depression: What Works, What to Avoid, and How to Stay Safe
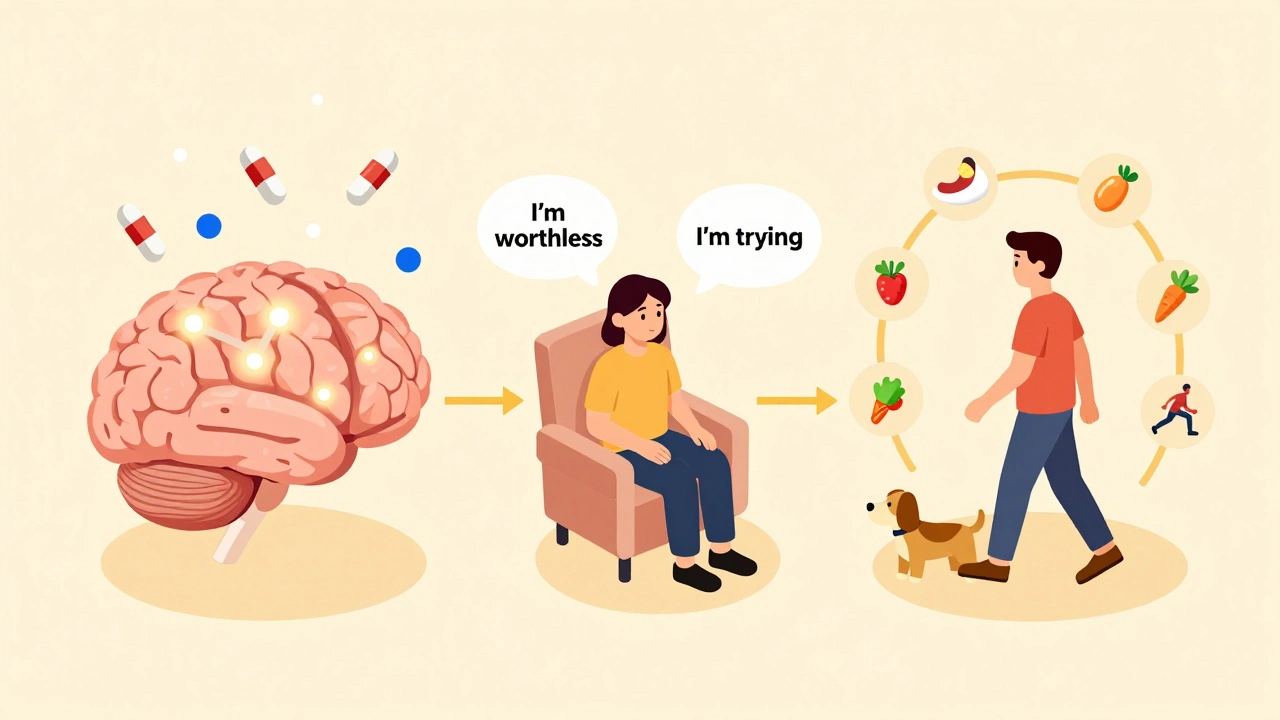
When it comes to therapy for depression, a range of medical and behavioral approaches used to reduce symptoms of persistent sadness, loss of interest, and impaired daily function. Also known as depression treatment, it can include medication, talk therapy, or a mix of both—depending on your needs and medical history. Many people assume antidepressants are the only answer, but that’s not true. The most effective plans often combine medication with changes in sleep, movement, and daily routine. What’s more, not all treatments are safe for everyone. For example, SSRIs, a class of antidepressants that increase serotonin levels in the brain to improve mood. Also known as selective serotonin reuptake inhibitors, they’re commonly prescribed but can carry risks during pregnancy or when mixed with other drugs. That’s why knowing the difference between a side effect and a true allergic reaction matters—something over half of patients get wrong.
Therapy for depression doesn’t start and end with a pill. It’s tied to how you manage your body and environment. Poor sleep, for instance, can make depression worse, and that’s why sleep hygiene, a set of daily habits that promote consistent, restful sleep without relying on medication. Also known as sleep habits, it’s one of the most underused tools in depression care. If you’re on multiple medications, you also need to watch for dangerous interactions. Statins, painkillers, or even common antibiotics can interfere with how your body processes antidepressants. And if you’re pregnant or planning to be, the risks of untreated depression can be greater than the risks of certain SSRIs—but only if you pick the right ones. That’s why a medication review, a structured check-up with your doctor or pharmacist to assess all your drugs for safety, effectiveness, and overlap. Also known as medicine checklist, it’s not optional if you’re on five or more prescriptions. Too many people skip this, then end up in the ER because of a hidden interaction.
You’ll find real stories here—not theory. Posts cover what happens when someone switches health plans and loses coverage for their antidepressant. They explain why generic drugs aren’t always interchangeable, even if they look the same. You’ll learn how to spot the early signs of a bad reaction, how to ask your pharmacist the right questions, and why some people need to monitor blood levels of their meds. There’s also guidance on what to do if you’re worried about long-term use, how to safely dispose of old pills, and how to avoid the trap of thinking more medication equals better results. This isn’t about pushing pills. It’s about helping you understand what’s actually working, what’s just noise, and how to stay in control of your treatment every step of the way.
Depression management combines medications, therapy, and lifestyle changes based on severity. SSRIs, CBT, exercise, and sleep hygiene are evidence-backed tools. Treatment is personalized-not one-size-fits-all.