Tumor Grades Explained: What Each Level Means for Treatment and Prognosis
When you hear tumor grades, a system pathologists use to classify how abnormal cancer cells look under a microscope. Also known as cancer differentiation, it tells doctors how fast a tumor is likely to grow and spread. It’s not the same as staging—which looks at size and spread—but it’s just as important. A low-grade tumor looks almost normal and grows slowly. A high-grade tumor looks wild, chaotic, and often spreads fast. Knowing the grade helps decide if you need chemo, radiation, or just close monitoring.
Tumor grades are usually measured on a scale from 1 to 4, sometimes labeled as G1 to G4. Grade 1 means the cells are well-differentiated—they still look like the tissue they came from. Grade 4 means they’re undifferentiated or poorly differentiated, barely recognizable as the original cell type. This isn’t just academic. A G3 or G4 tumor often needs more aggressive treatment, even if it’s small. For example, a Grade 3 breast tumor might need chemo even if it hasn’t spread to lymph nodes, while a Grade 1 might not. The same applies to brain tumors, prostate cancer, and sarcomas. Pathologists look at cell shape, nucleus size, and how organized the tissue is. No two tumors are exactly alike, but the grading system gives doctors a common language to talk about risk.
Grading relies on biopsy samples, so accuracy matters. Sometimes, different pathologists might assign slightly different grades—this is why second opinions are common in cancer care. It’s also why some tumors are regraded after surgery, when more tissue is available. A tumor that looked like Grade 2 on a needle biopsy might turn out to be Grade 3 after full removal. That change can shift treatment plans. And it’s not just about the grade. Grade often works with other factors: tumor size, gene mutations, hormone receptors, and whether it’s invaded nearby tissue. But if you’re trying to understand your diagnosis, start with the grade. It’s the clearest signal of how aggressive your cancer is.
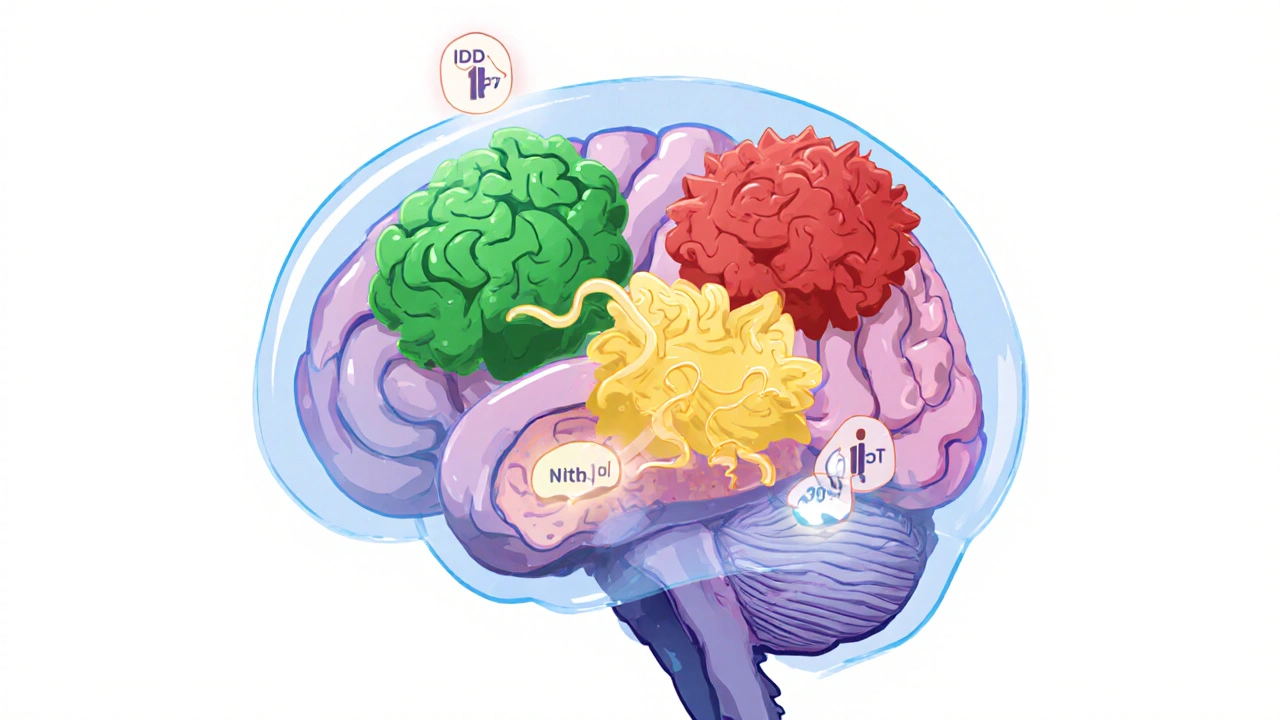
Some cancers use different systems. Prostate cancer uses the Gleason score, which combines two patterns into a number. Brain tumors use the WHO classification, which includes molecular markers. But the core idea stays the same: how abnormal do the cells look, and what does that mean for behavior? High-grade tumors don’t always mean death—they just mean you need to act faster. Low-grade doesn’t mean safe—it means you need to stay vigilant. The goal isn’t to scare you, but to give you real information so you can ask the right questions.
Below, you’ll find real-world comparisons and deep dives into how tumor grades affect treatment choices across different cancers—from breast and prostate to brain and liver. You’ll see how grading impacts everything from drug selection to survival odds. No fluff. Just what you need to understand your diagnosis and talk confidently with your care team.
Understand brain tumor types, WHO CNS5 grading, and modern treatments including vorasidenib and molecular diagnostics. Learn how IDH mutations and 1p/19q codeletion impact survival and therapy choices.