Left Ventricular Dysfunction's Impact on Kidney Function
So, you've probably heard that the heart and kidneys are best buddies when it comes to keeping the body running smoothly. But what happens when the heart isn't in tip-top shape, especially the left ventricle? Well, it isn't just a heart problem—it can ripple out and hit those hard-working kidneys too.
Firstly, let's talk about left ventricular dysfunction. This is when the left ventricle (basically the heart's main squeeze) doesn't pump blood as efficiently as it should. This can lead to less oxygen-rich blood making its way around the body, including the kidneys. And when kidneys don't get enough blood, they can't filter waste properly, which is a bit of a kick in the teeth for your overall health.
This connection between heart and kidney means they've got to be treated like a pair. If your left ventricle isn't working right, it's not just about dealing with heart issues anymore. There's a bigger picture involving your kidneys that needs attention. Recognizing symptoms early, like fatigue and swelling in legs or feet, could help you catch potential kidney issues sooner rather than later.
Stick around as we dive into more detail about how these two systems play together and what you can do to keep both your heart and kidneys on the right track.
- Basic Understanding of Left Ventricular Dysfunction
- Heart-Kidney Connection
- Impact on Kidney Function
- Managing Health Concerns
Basic Understanding of Left Ventricular Dysfunction
Let's break down this big phrase: left ventricular dysfunction. It sounds fancy, but at its core, it's all about how well the left ventricle of your heart does its job. The left ventricle is like the heart's powerhouse. It's responsible for pumping oxygen-rich blood from your heart to the rest of your body. When it's not working as it should, that's when we talk about left ventricular dysfunction.
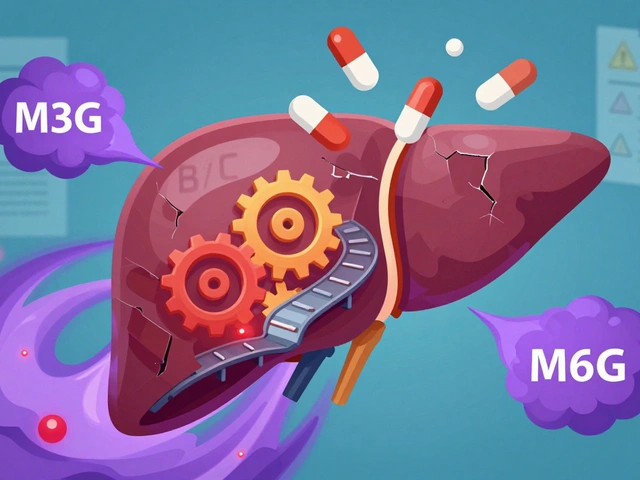
There are two main types of dysfunction you might hear about: systolic and diastolic. In systolic dysfunction, the left ventricle can’t contract properly, which means it doesn't push out enough blood. Imagine trying to squeeze a sponge that doesn’t press down all the way—same idea. Diastolic dysfunction, on the other hand, is when the ventricle doesn’t fill up with enough blood. It's like a sponge that can’t soak up water properly.
Causes and Symptoms
Common causes of these dysfunctions include coronary artery disease, high blood pressure, and heart attacks. It's like too much strain and pressure on the heart’s streets and highways! When these happen, the heart can't maintain its normal function, leading to a chain reaction of other issues.
As for symptoms, if you're feeling short of breath, exceptionally tired, or notice swelling in your legs, these could be signs of left ventricular dysfunction. It's basically your body giving you a not-so-subtle nudge to get checked out.
Diagnosis and Treatment
Diagnosis often involves a few tests. You'll likely hear about an echocardiogram, which is basically an ultrasound for your heart, giving docs a good look at how your heart's doing.
- Medication: Drugs like ACE inhibitors, beta-blockers, and diuretics often get prescribed to help manage symptoms and improve heart function.
- Lifestyle Changes: Eating right, exercising, and cutting back on salt can help lighten the load on your heart.
Being proactive with these measures helps keep symptoms in check and improves quality of life. Remember, talking to your doctor about any of these symptoms is crucial; early intervention can make all the difference.
Heart-Kidney Connection
The relationship between the heart and kidneys is like the ultimate example of teamwork. When everything's working smoothly, the heart pumps blood, the kidneys filter waste, and life goes on without a hitch. But with left ventricular dysfunction, things can get tricky.
Basically, when the left ventricle isn't pumping efficiently, the kidneys can't do their job properly. You see, they rely on that steady flow of blood to filter out waste and balance fluids. If blood flow drops or is inconsistent, the kidneys start feeling the pressure. This can make you prone to fluid retention, further stressing other organs.
Why This Matters
The heart and kidneys work in tandem, and when one struggles, the other often follows. Over time, this can lead to chronic kidney disease, making managing both conditions way more challenging. If you're dealing with heart issues, knowing this connection can help you spot potential kidney problems sooner.
| Condition | Impact on Kidneys |
|---|---|
| Left Ventricular Dysfunction | Reduced blood flow reduces kidney function |
| Chronic Heart Failure | Fluid retention affects kidney workload |
Spotting the symptoms can make a huge difference. Look out for things like swelling in your ankles, unexplained fatigue, or difficulty breathing. These could be signs that your kidneys are struggling because of kidney function.
In short, understanding this heart-kidney duo helps you take control of your health, nipping problems in the bud and keeping both your heart and kidneys happy.
Impact on Kidney Function
When we talk about left ventricular dysfunction, the heart's impaired ability to pump blood effectively isn't just its own problem. This inefficiency can really create a domino effect, particularly when it comes to kidney function.
The Blood Flow Issue
Think about it: if your heart's having trouble keeping the blood flow strong and steady, your kidneys are going to notice. These hardworking organs rely heavily on a consistent blood supply to do their job of filtering out waste and excess fluids. With less blood reaching the kidneys, their efficiency drops, which can lead to a whole host of issues, including fluid retention and electrolyte imbalances.
Kicking In Other Problems
And it doesn't stop there. Left ventricular dysfunction can increase the risk of developing chronic kidney disease (CKD). If your kidneys are underperfused for a long time, it starts a cycle that can be tough to break. We often see elevated creatinine levels as a warning sign—your kidneys aren't clearing out waste like they're supposed to, leaving all that extra stuff swirling around in your system.
Some studies have suggested that about 50% of patients with heart failure will experience some level of kidney dysfunction—yeah, those numbers are pretty telling. It's kind of like how ignoring a small leak is bound to cause bigger plumbing problems down the road.
| Condition | Percentage of Patients |
|---|---|
| Heart Failure with Kidney Dysfunction | 50% |
Keeping a Check
Tackling these issues means being proactive. Regular check-ups are key. If you're dealing with left ventricular dysfunction, keeping an eye on kidney health involves regular blood tests to monitor functioning. It's also wise to talk with your healthcare provider about integrating specialists who focus on both heart and renal impact to make sure your whole body's getting the attention it deserves.
Overall, understanding how intertwined these systems are can make a big difference in treating not just the heart but ensuring your kidneys aren't left in the lurch. Remember, your body's a team, and when one player's down, it needs all the support it can get!
Managing Health Concerns
When you're dealing with left ventricular dysfunction, leaving your health to chance ain't a great strategy. It's all about being proactive, especially since both your heart and kidney function are in the mix.
Regular Check-Ups
Don't skip those doctor visits. Keeping tabs on your blood pressure, heart rate, and kidney function can literally be a lifesaver. Catching any changes early makes a huge difference. Ask your healthcare provider about specific tests to monitor your condition closely.
Medication Management
Whether it's blood pressure meds, diuretics, or special pills to support your heart, sticking to your medication schedule is crucial. It can keep your symptoms in check and prevent additional issues down the road. If you have side effects, have a chat with your doctor about alternatives or adjustments.
Healthy Lifestyle Choices
The pep talk about eating better and moving more isn't just fluff. A heart-healthy diet can also support your kidneys. Focus on:
- Eating more fruits and veggies.
- Cutting back on salt.
- Choosing lean proteins.
Keep up with some form of physical activity too. Even a daily walk can improve blood circulation and help manage weight.
Stay Hydrated, Within Limits
It's a bit of a balancing act. While you want to stay hydrated, be mindful of fluid intake if your doc advises it due to kidney concerns. Dehydration or overhydration can complicate things.
Emotional and Mental Health
Remember, stress isn't your friend in this scenario. Managing stress through meditation, hobbies, or even chatting with a friend can keep your mind as healthy as your body.
Keep these all in mind, take one step at a time, and you'll be better equipped to tackle the challenges that come with left ventricular dysfunction.





Comments (19)
Karen Ballard
25 Mar 2025
Great overview, thanks! 👍
Gina Lola
26 Mar 2025
The hemodynamic repercussions of reduced left ventricular output manifest as compromised renal perfusion, which in turn triggers neurohormonal activation. When the glomerular filtration rate drops, the renin‑angiotensin‑aldosterone system kicks into overdrive, aggravating fluid retention. This feedback loop is a classic cardio‑renal syndrome scenario. Bottom line: keep an eye on both heart and kidney metrics.
Leah Hawthorne
27 Mar 2025
I’ve seen patients where the heart‑kidney axis really dictates the clinical course. Once the left ventricle starts faltering, the kidneys quickly feel the pressure because they rely on steady perfusion. Even mild reductions in ejection fraction can push creatinine upward over weeks. That’s why routine labs become essential, not just imaging. Also, managing blood pressure aggressively can buy time for both organs. It’s a team sport, and the doctor’s job is to coordinate that team.
Brian Mavigliano
28 Mar 2025
But let’s not romanticize the kidney as a passive victim. The renal system has its own autoregulatory mechanisms that can buffer short‑term drops in flow. If we over‑medicate with diuretics just to protect the heart, we might blunt that protective response. So the therapeutic balance isn’t as straightforward as “fix the heart, the kidneys will follow.” A nuanced approach is required.
Emily Torbert
29 Mar 2025
Totally get how overwhelming this can feel “just take your meds and walk” isn’t always that easy though
Rashi Shetty
30 Mar 2025
While the lay perspective often simplifies the pathophysiology, it is imperative to acknowledge the intricate interplay of neurohormonal cascades and endothelial dysfunction that accompanies left ventricular deterioration. Evidence suggests that early intervention with ACE inhibitors can mitigate renal compromise, thereby preserving glomerular filtration rates. Monitoring serum electrolytes and creatinine at regular intervals remains a cornerstone of comprehensive care. 🚑
Queen Flipcharts
31 Mar 2025
In the context of American medicine, the emphasis on multidisciplinary clinics exemplifies our commitment to tackling such intertwined conditions. Our hospitals are equipped with both cardiology and nephrology teams working under one roof, ensuring seamless communication. This model should serve as a benchmark for other nations striving to improve patient outcomes. Ignoring the cardio‑renal connection would be a disservice to our citizens.
Yojana Geete
1 Apr 2025
OMG, the drama between the heart and kidneys is like a soap opera you can't stop watching! One minute the heart's all dramatic and the kidneys are like “help me!”, next thing you know there's fluid everywhere 😱
Jason Peart
2 Apr 2025
Hey folks, let’s break this down step by step so nobody feels lost.
First off, the left ventricle is the powerhouse that sends oxygen‑rich blood to every organ, kidneys included.
When its pumping strength drops, the kidneys notice fast because they need a steady flow to yank waste out of the blood.
That drop in flow triggers the body’s emergency response, releasing hormones like renin and angiotensin that try to keep the pressure up.
Unfortunately, those same hormones make the blood vessels leaky and cause the body to hold onto extra fluid.
The extra fluid then piles up in the legs, lungs, and even the kidneys, making them work harder.
Over time this extra workload can scar the tiny filtering units called nephrons, and that’s when you start seeing a rise in creatinine.
The good news is that we have a toolbox of meds – ACE inhibitors, ARBs, beta‑blockers – that can help both the heart and the kidneys at the same time.
It’s also vital to keep an eye on your blood pressure, because high pressure is a double‑edged sword for both organs.
Regular labs, like a basic metabolic panel, let your doc see trends early before things get out of hand.
Lifestyle changes matter too – cutting down on sodium, moving a bit each day, and staying within your fluid limits if your doc says so.
Even small things like sitting up after meals can reduce the strain on the heart‑kidney circuit.
If you ever feel dizzy, unusually short of breath, or notice your shoes feeling tighter, that could be a sign the system is crying out for help.
Don’t wait for an emergency room visit; call your healthcare team and get checked.
Remember, you’re not alone in this – there are support groups, online forums, and community resources ready to back you up.
Stay proactive, stay positive, and give your body the respect it deserves.
Hanna Sundqvist
3 Apr 2025
Honestly, think about how pharma pushes diuretics just to keep us dependent, while the real fix is hidden in the data they don’t want us to see.
Jim Butler
4 Apr 2025
Let’s turn this challenge into an opportunity! 💪 Consistent monitoring, adherence to therapy, and a proactive mindset can dramatically improve outcomes. Stay focused and trust the process. 🌟
Ian McKay
5 Apr 2025
The sentence structures in the previous comment could benefit from clearer punctuation; for instance, a semicolon might replace the comma to separate independent clauses. Additionally, “its” should be “it’s” when denoting “it is.” Proper syntax enhances readability.
Deborah Messick
6 Apr 2025
While many celebrate the notion of a seamless cardio‑renal interface, the reality is that clinical guidelines often overlook subtle individual variations. A one‑size‑fits‑all protocol may inadvertently neglect patients with atypical presentations, thereby compromising care quality.
Jolanda Julyan
7 Apr 2025
I must say that the argument presented earlier seems a bit shallow.
The heart and kidney relationship is not just a simple cause and effect.
There are many layers of physiology that need to be considered.
For example, the role of sympathetic nervous system activation cannot be ignored.
Also, the impact of chronic inflammation on both organs is well documented.
Ignoring these factors leads to incomplete treatment plans.
Doctors should therefore order comprehensive panels, not just basic tests.
Lifestyle interventions must be tailored to each patient’s unique circumstances.
A diet low in sodium but rich in potassium can benefit both heart and kidneys.
Regular aerobic exercise improves vascular compliance, aiding perfusion.
Patient education empowers individuals to recognize early warning signs.
In conclusion, a holistic approach is essential for optimal outcomes.
Kevin Huston
8 Apr 2025
The data clearly paints a picture of systemic failure when the left ventricle sputters; it’s a cascade of dysregulated cascades, a veritable domino effect that drags the kidneys into the abyss of dysfunction.
Amanda Hamlet
9 Apr 2025
Actually, you’re all missing the point – the pharmacogenomics of ACE inhibitors dictate individual response, and without genotype testing you’re basically guessing.
Nolan Jones
10 Apr 2025
From a practical standpoint, I always start patients on low‑dose ACE inhibitors and titrate up while monitoring potassium. If the eGFR drops more than 30% from baseline, I reassess immediately. Pairing that with a modest loop diuretic can control fluid overload without over‑taxing the kidneys. Also, encourage a sodium intake under 2 grams per day and a daily walk of at least 20 minutes. This regimen has helped many of my patients maintain stable renal function while improving cardiac output.
Jada Singleton
11 Apr 2025
The previous suggestion is overly simplistic and neglects the nuanced interplay of vasoactive substances; such an approach risks iatrogenic harm.
Emily Rossiter
12 Apr 2025
Keep pushing forward, and remember that small consistent steps add up to big health gains.