Steroid Use and Osteoporosis Risk: What You Need to Know

Steroid Osteoporosis Risk Calculator
Estimate Your Osteoporosis Risk
This tool estimates your fracture risk based on steroid use and other factors. Results are for informational purposes only and should not replace medical advice.
Your Risk Assessment
Recommended Actions
Key Takeaways
- Glucocorticoids are the #1 drug‑induced cause of osteoporosis.
- Even low‑dose, short‑term steroids can lower bone mineral density (BMD).
- Risk climbs with age, female sex, smoking, and previous fractures.
- DXA scans should be done before starting chronic steroids and repeated yearly.
- Calcium, vitaminD, weight‑bearing exercise, and sometimes bisphosphonates keep bones strong while you need steroids.
When doctors prescribe Glucocorticoids synthetic steroids that reduce inflammation, they’re often focused on the short‑term benefit-pain relief, immune suppression, or control of autoimmune disease. What many patients overlook is the silent side‑effect that creeps in months later: bone becomes porous, fractures become more likely. This article lays out how steroids damage bone, who should be most worried, and practical steps to protect your skeleton without abandoning the medication you need.
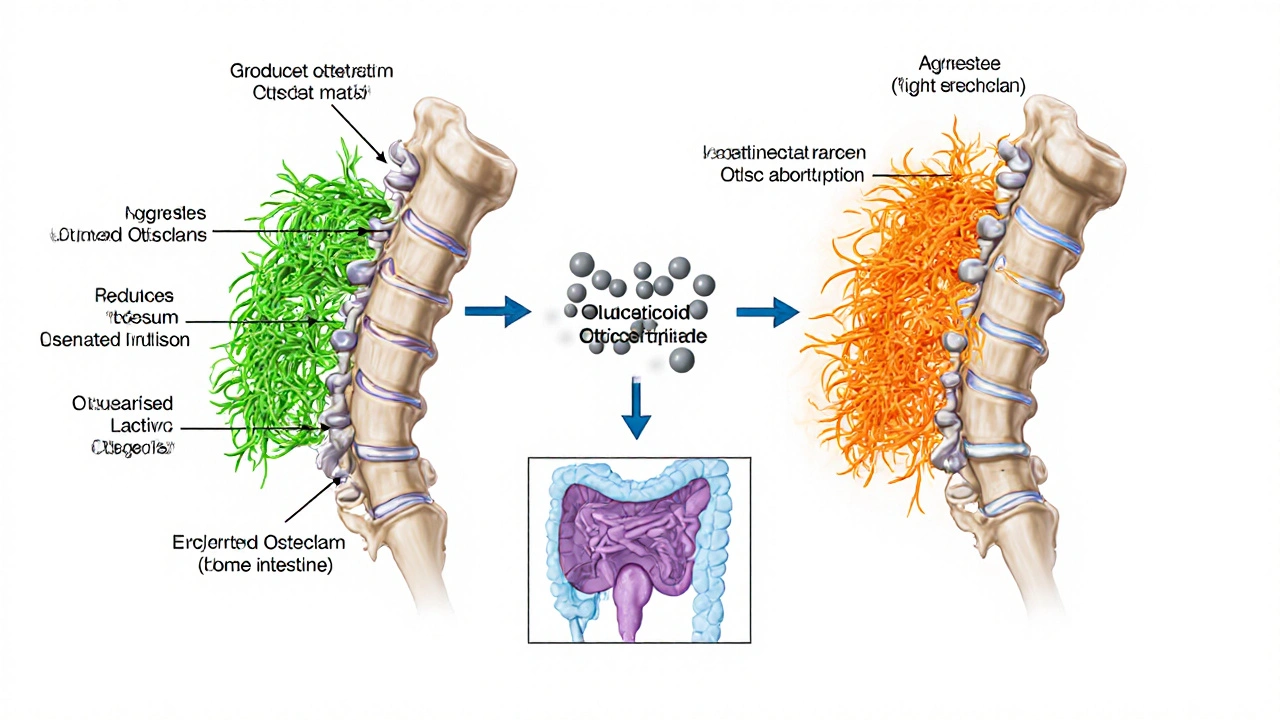
How Steroids Attack Bone
Bone is a living tissue that constantly remodels-cells called osteoclasts break down old bone, while osteoblasts lay down new matrix. Glucocorticoids tip this balance in three ways:
- Osteoblast suppression: Steroids cut the production of collagen and alkaline phosphatase, the building blocks osteoblasts need.
- Osteoclast activation: They increase the lifespan of osteoclasts, so more bone gets resorbed.
- Calcium handling: Steroids reduce calcium absorption in the gut and increase calcium loss via the kidneys, prompting the parathyroid gland to release more PTH, which further drives bone loss.
Within the first three months of daily prednisone≥5mg, patients can lose up to 2‑3% of BMD at the lumbar spine-roughly the amount lost in a year of natural aging.
Who Is Most at Risk?
Not everyone on steroids will develop osteoporosis, but certain factors magnify the danger:
- Age: People over 65 have slower bone formation, so steroids hit harder.
- Sex: Women, especially post‑menopausal, lose estrogen‑driven bone protection.
- Baseline BMD: Low Bone Mineral Density (a measurement of bone strength) before therapy predicts steeper declines.
- Dosage & duration: Cumulative dose >1g of prednisone equivalents over a year markedly raises fracture odds.
- Lifestyle: Smoking, heavy alcohol, and sedentary habits already erode bone.
- Comorbidities: Rheumatoid arthritis, chronic kidney disease, and malabsorption syndromes add extra risk.
Spotting Bone Loss Early
The gold standard for diagnosing steroid‑induced bone loss is the DXA Scan (dual‑energy X‑ray absorptiometry). It measures BMD at the lumbar spine and hip, giving a T‑score that compares you to a healthy 30‑year‑old.
Guidelines suggest:
- Perform a baseline DXA before starting < 3months of daily glucocorticoids if you’re over 40 or have other risk factors.
- Repeat the scan annually for anyone on steroids for ≥3months.
- Watch for “silent” vertebral fractures-often discovered only on lateral spine X‑ray after back pain.
Practical Ways to Guard Your Bones
Even if you can’t ditch the steroid, you can stack strategies that blunt the bone‑damage cascade.
1. Calcium & VitaminD
Calcium 1,000‑1,200mg per day (1,200mg if over 50) and vitaminD800‑1,000IU are the foundation. VitaminD improves gut calcium absorption, counteracting the steroid‑induced drop.
2. Weight‑Bearing Exercise
Activities that stress the skeleton-walking briskly, stair climbing, resistance bands, or light weightlifting-stimulate osteoblast activity. Aim for 150minutes of moderate‑intensity activity weekly, plus two strength sessions.
3. Smoking Cessation & Alcohol Moderation
Quitting smoking can restore bone turnover rates within a year. Limit alcohol to ≤2units per day for men and ≤1unit for women.
4. Pharmacologic Protection
When risk exceeds a 3% 10‑year major osteoporotic fracture probability (FRAX score), consider medication.
| Intervention | Mechanism | Typical Dose / Frequency | Evidence Level |
|---|---|---|---|
| Calcium | Provides mineral substrate for bone matrix | 1,000‑1,200mg daily | Strong |
| VitaminD | Enhances intestinal calcium absorption | 800‑1,000IU daily | Strong |
| Bisphosphonates (e.g., alendronate) | Inhibit osteoclast‑mediated bone resorption | 70mg weekly or 5mg daily for 30days | Very Strong |
| Teriparatide | Recombinant PTH1‑34 stimulates osteoblasts | 20µg subcut daily | Strong (for high‑risk patients) |
| Denosumab | Monoclonal antibody that blocks RANKL, reducing osteoclast activity | 60mg SC every 6months | Strong |
Bisphosphonates are usually first‑line because they’re cheap, oral, and have decades of data showing fracture risk reduction in steroid‑treated patients.
5. Timing Matters
Start calcium, vitaminD, and any bone‑protective drug within two weeks of initiating steroids. If steroids are tapered quickly (≤3months total), some clinicians opt for just supplements and close monitoring.

Managing Existing Osteoporosis While Still on Steroids
If you already have a diagnosis of osteoporosis, the goal shifts to halting further loss and rebuilding bone.
- Continue bisphosphonate therapy for at least three years before reassessing the need to pause.
- Consider switching to a bone‑forming agent like teriparatide if you’ve suffered a vertebral fracture on a bisphosphonate.
- Re‑evaluate BMD with DXA after 12‑18months of combined therapy.
- Engage a multidisciplinary team-rheumatologist, endocrinologist, physiotherapist-to balance disease control and bone health.
Importantly, never stop steroids abruptly; taper under medical supervision to avoid adrenal insufficiency.
Quick Checklist for Patients on Steroids
- Ask your doctor for a baseline DXA before starting long‑term steroids.
- Take calcium 1,200mg + vitaminD1,000IU daily.
- Fit in at least 30minutes of weight‑bearing activity, five days a week.
- Quit smoking and limit alcohol.
- If you’re 40+ or have other risk factors, discuss starting a bisphosphonate.
- Schedule a follow‑up DXA after 12 months.
Frequently Asked Questions
Can short courses of steroids cause osteoporosis?
Even a 2‑week burst of prednisone≥10mg daily can trigger a modest dip in calcium balance, but measurable BMD loss usually requires continuous exposure for at least 3months. Still, if you have other risk factors, a brief DXA check can be reassuring.
Is calcium alone enough to protect my bones?
Calcium is essential, but without adequate vitaminD it isn’t absorbed well. Moreover, steroids still accelerate bone resorption, so most high‑risk patients need a second line agent like a bisphosphonate.
Are there any steroids that are safer for bone?
The risk correlates with glucocorticoid potency, not the specific drug. Low‑dose inhaled steroids for asthma have minimal systemic absorption and thus low bone impact, whereas oral or IV formulations carry the highest risk.
What is the FRAX score and do I need it?
FRAX estimates your 10‑year probability of a major osteoporotic fracture using age, sex, weight, height, previous fractures, glucocorticoid use, and more. If you’re on chronic steroids, your doctor will likely run FRAX to decide if medication beyond supplements is warranted.
Can exercise reverse bone loss caused by steroids?
Weight‑bearing exercise can stimulate new bone formation, but it won’t fully counteract the rapid resorption caused by high‑dose steroids. It works best when paired with calcium, vitaminD, and possibly a bisphosphonate.
Understanding the link between osteoporosis and steroid therapy empowers you to ask the right questions, plan preventative steps, and keep fractures at bay while still benefiting from the medication that controls your underlying condition.





Comments (19)
April Rios
14 Oct 2025
Steroid therapy, especially long‑term glucocorticoids, is a silent architect of bone loss.
The glucocorticoid receptor on osteoblasts shuts down the very genes that build new matrix.
At the same time, it fuels osteoclast activity, turning the remodeling balance toward resorption.
Age amplifies this effect because the adaptive capacity of the skeletal system wanes after the fifth decade.
Women, particularly post‑menopausal, carry an additional hormonal deficit that predisposes them to fractures.
Dose matters; each incremental milligram of prednisone equivalent compounds the micro‑damage in a roughly linear fashion.
Duration is the hidden multiplier-six months of 10 mg is not the same as a single high‑dose burst.
Smoking introduces oxidative stress that further erodes trabecular connectivity.
A prior fracture is a biological footnote that the skeleton has already failed to heal, signalling a compromised architecture.
Calcium and vitamin D intake act as the only modifiable nutrients that can partially offset glucocorticoid‑induced calcium loss.
Weight‑bearing exercise, even in modest amounts, stimulates mechanotransduction pathways that can blunt the catabolic signal.
Bisphosphonates and denosumab have emerged as pharmacologic anchors for those who cannot wean off steroids.
However, these agents come with their own risk profile, demanding a shared decision‑making process with the clinician.
The calculator you linked is a heuristic, not a definitive prognosis; it aggregates risk but cannot predict the timing of an individual fracture.
Ultimately, the prudent strategy is to use the lowest effective steroid dose for the shortest feasible period while instituting bone‑protective measures from day one.
In practice, that means regular DEXA scans, lifestyle counseling, and a low threshold for prophylactic therapy.
Remember that the skeletal system is a living organ; its health reflects the sum of endocrine, nutritional, and mechanical inputs over a lifetime.
Ignoring any one of those inputs in the presence of steroids is akin to building a house on sand.
So treat the calculator as a conversation starter, not a verdict, and let the data guide a comprehensive bone health plan.
byron thierry
14 Oct 2025
Your observation that dosage and duration are critical aligns with the endocrine literature. While the calculator simplifies complex physiology, it remains a valuable screening tool. Clinicians should interpret the output in the context of patient‑specific risk factors. The recommendation for calcium, vitamin D, and possible bisphosphonate therapy is well founded.
M Black
14 Oct 2025
lol steroids can mess up your bones 😬 but if you keep moving and get some sunshine it ain't the end of the world 🎉
Sidney Wachira
14 Oct 2025
Behold! The silent thief that lurks in every prednisone pill! 😱 It strikes when you least expect it, leaving your skeleton in ruins!
Julie Sook-Man Chan
14 Oct 2025
I appreciate the detailed breakdown. It helps me understand my own risk better.
Amanda Mooney
14 Oct 2025
Great summary! This gives me confidence to discuss prophylaxis with my doctor.
Mandie Scrivens
14 Oct 2025
Oh sure, just another calculator to ruin my day. Thanks for the joy.
Richa Ajrekar
14 Oct 2025
The article is, admittedly, lacking in citation. Nevertheless, the core message is conveyed.
Pramod Hingmang
14 Oct 2025
I hear you, steroid therapy feels like a double‑edged sword. You’re juggling pain relief and bone health, a tough act. Keep pushing, every step counts.
Michael Barrett
14 Oct 2025
One could argue that steroids are the modern Prometheus, gifting relief while stealing bone strength. The paradox lies not in the drug but in our stewardship of its use. Therefore, risk calculators serve as mirrors, reflecting our dosing choices. Ignoring them is tantamount to hubris.
Inma Sims
14 Oct 2025
Indeed, the calculator's output is as definitive as a fortune‑cookie. Yet, it does provide a scaffolding for discussion. Let us not mistake scaffolding for the finished edifice.
Gavin Potenza
14 Oct 2025
The bone, like the mind, responds to pressure and neglect. In the context of glucocorticoids, we observe a forced adaptation that may become maladaptive. Reflecting on this, one might reconsider the balance between therapeutic benefit and skeletal cost. Ultimately, wisdom resides in measured use.
Virat Mishra
14 Oct 2025
Wow steroids ruin everything. It's just another health nightmare.
Frank Pennetti
14 Oct 2025
From a pharmacoeconomic perspective, the cost‑benefit analysis of prophylactic bisphosphonates versus fracture morbidity is statistically significant. Hence, protocol optimization is non‑negotiable.
Adam Baxter
14 Oct 2025
Stay active and get your DEXA scan.
Keri Henderson
14 Oct 2025
You’ve got this, just follow the bone‑health checklist. Prioritize calcium, vitamin D, and weight‑bearing exercise.
elvin casimir
15 Oct 2025
Honestly, the writing could use some proof‑readin. It's full of common gramer mistakes. Please fix it.
Steve Batancs
15 Oct 2025
Your sarcasm misses the point entirely.
Ragha Vema
15 Oct 2025
They don’t want you to know that pharma hides the true bone‑loss data. The calculator is just a smoke screen, a diversion from the real agenda. Wake up and demand transparency!