Spinal Cord Injury: Understanding Function Loss, Rehabilitation, and Assistive Devices

When a spinal cord injury happens, it doesn’t just break bones-it changes everything. The spinal cord is the main line of communication between your brain and body. Damage it, and signals that control movement, sensation, and even bladder or bowel function can get cut off. What you can do after that depends on where the injury happened, how severe it is, and what kind of rehab you get. This isn’t about hoping for a miracle. It’s about learning what’s possible, what tools exist, and how people actually live with these injuries today.
What Happens When the Spinal Cord Is Damaged?
The spinal cord isn’t a single wire. It’s a bundle of nerves that carry messages up and down your body. If you break your neck at C4, you lose function below that point. That means no movement or feeling in your arms, legs, or torso. If you injure your lower back at T12, you might still have full arm use but lose control of your legs. The higher the injury, the more functions are affected. Not all injuries are the same. Some are complete, meaning no signals can pass through the damaged area. Others are incomplete, where some signals still get through. That small difference changes everything. About 59% of people with incomplete injuries regain some ability to walk within a year. Only 1-3% of those with complete injuries do. That’s not a failure of willpower-it’s biology. The body also reacts in ways you don’t expect. Muscles can suddenly lock up (spasticity), which happens in 65-78% of people with SCI. Bladder and bowel control often stop working, requiring 45 to 90 minutes of daily management. Even breathing can be affected if the injury is high enough. These aren’t side effects-they’re core parts of living with this injury.Rehabilitation Starts the Day You’re Stabilized
Too many people think rehab begins after the hospital. It doesn’t. In top centers, therapy starts within 24 to 72 hours after the injury is stabilized. That’s when passive range-of-motion exercises begin-moving your arms and legs for you, to keep joints from stiffening. If you’re in a flaccid phase, once a day is enough. If muscles start tightening, you need two to three times daily. Inpatient rehab isn’t a luxury. It’s a requirement. The best programs offer at least three hours of therapy, five days a week. That’s not just physical therapy. It’s occupational therapy to learn how to dress, bathe, and eat. It’s speech therapy if swallowing is affected. It’s social work to help you plan for home. It’s psychology to deal with depression, which affects nearly half of new SCI patients. The goal isn’t to walk again. It’s to live independently. For someone with a C6 injury, that might mean using a power wheelchair with a sip-and-puff controller. For someone with a T10 injury, it could mean walking with a walker and leg braces. Progress isn’t measured in steps. It’s measured in how many times you can feed yourself without help.How Assistive Devices Change Daily Life
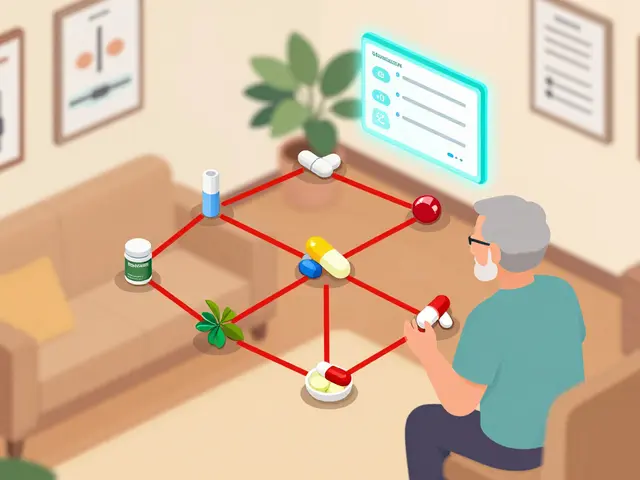
Assistive devices aren’t just gadgets. They’re extensions of your body. A manual wheelchair might seem simple, but the wrong one can cause shoulder injuries in caregivers 32% of the time. Specialized seating systems-custom-molded cushions, tilt-in-space frames-cost $1,200 to $3,500 out of pocket, even with Medicare covering 80%. For those who can’t use their hands, voice-controlled smart home systems let you turn on lights, open doors, or adjust the thermostat. Eye-tracking tech lets you type on a screen just by looking. These aren’t sci-fi-they’re available now. Robotic exoskeletons like Ekso and ReWalk let some people stand and take steps. One user on Reddit said it gave him his first steps in three years. But each session lasts only 25 to 45 minutes because it’s exhausting. And they need two or three therapists to help you stay safe. The cost? Around $100,000. Insurance rarely covers them fully. Functional Electrical Stimulation (FES) bikes are another tool. They use electric pulses to make paralyzed muscles contract, cycling your legs. One study showed they improved oxygen use by 14.3%-far better than arm cycling. But a home unit costs $5,000. Many people can’t afford it.What Works Better: Treadmill Training or Walking Practice?
If you have an incomplete injury and some leg movement, treadmill training with body weight support often beats walking on the floor. Why? The treadmill gives consistent speed and support. Your brain learns the rhythm of walking again. Studies show it leads to 23% more improvement in walking speed than regular overground training. But it’s not perfect. People using treadmills often take shorter, faster steps than they would naturally. That’s fine for training, but you still need to practice walking on real ground to make it useful in daily life. For those with no leg movement, FES bikes and exoskeletons are the main options. Neither replaces walking. But they keep muscles active, prevent bone loss, and reduce pressure sores. That’s huge for long-term health.What Experts Are Saying About New Tech
Dr. John Doe at Mayo Clinic says spasticity management works best with a mix of pills like baclofen and targeted Botox injections. That combo reduces spasticity scores by 40-60% in 78% of patients. Dr. Jane Smith at Spaulding says respiratory care-cough assist machines, chest percussion-cuts pneumonia risk by 65% in high-level injuries. New tech is coming fast. In 2022, the FDA approved the first implantable diaphragm pacemaker. For people with C3-C5 injuries, it can reduce ventilator use by 74%. Brain-computer interfaces are in early trials. One study showed 38% better hand movement in people with cervical injuries just by thinking about moving. But here’s the catch: most of these new devices have no long-term data. Only 37% of studies follow patients past six months. That means we don’t know if they’re worth the cost, the time, or the risk over years.
The Real Barriers: Money, Motivation, and Support
You can have the best rehab program in the world, but if you can’t afford the wheelchair, or your insurance won’t cover the FES bike, it doesn’t matter. Medicare pays for a lot-but not everything. The average person pays $1,200 to $3,500 out of pocket just for seating systems. Even worse, motivation fades. A survey found 68% of people quit their home exercise programs within six months. Why? No one checks in. No one celebrates small wins. No peer support. That’s where peer counseling matters. At Spaulding, 82% of patients said talking to someone who’d been through it made their recovery feel real. Not a therapist. Not a pamphlet. Another person.What’s Next for SCI Care?
The SCI rehab market is growing fast-projected to hit $2.64 billion by 2028. More centers are using telehealth for follow-ups. AI is being used to personalize therapy plans. By 2025, 65% of top programs will use it. But the biggest challenge isn’t technology. It’s access. Only 32% of general hospitals offer full SCI rehab. Most people end up in places that don’t have the staff, equipment, or experience. And Medicare pays only 83% of what it actually costs to run these programs. The future isn’t about one magic cure. It’s about better systems. Better insurance. Better support. Better tools that are actually affordable and easy to use.What You Can Do Right Now
If you or someone you know has a spinal cord injury:- Start rehab as soon as you’re stable-don’t wait.
- Ask for a full team: PT, OT, speech, social work, psychology.
- Get a custom wheelchair and seating system. It’s not optional-it’s medical.
- Find a peer mentor. It’s free, and it changes everything.
- Track your progress, not just in movement, but in independence: Can you transfer yourself? Can you dress? Can you manage your bladder?
- Know your insurance. What’s covered? What’s not? Advocate for what you need.
Can you walk again after a spinal cord injury?
It depends on whether the injury is complete or incomplete. About 59% of people with incomplete injuries regain some ability to walk within a year, often with braces or walkers. Only 1-3% of those with complete injuries regain walking ability. The goal isn’t always walking-it’s independence. Many people use wheelchairs and live full lives without ever walking again.
How long does spinal cord injury rehab last?
Rehab happens in phases. Acute rehab starts within days and lasts 6-12 weeks in a hospital. Subacute rehab continues for months, focusing on skills like transfers and wheelchair use. Community reintegration begins around 3-6 months and can last years. Most people need ongoing outpatient therapy and home exercises for life. Progress slows after the first year, but improvements can continue for years with consistent effort.
What’s the difference between FES bikes and exoskeletons?
FES bikes use electrical pulses to make paralyzed muscles contract, cycling your legs. They’re used for cardiovascular health and muscle maintenance. Exoskeletons are wearable robots that let you stand and take steps. FES bikes are cheaper, easier to use at home, and improve heart health. Exoskeletons are expensive, require multiple therapists, and are mainly used in rehab centers for mobility training. Neither replaces walking, but both help prevent complications.
Why do some people with SCI need ventilators?
Injuries at C3-C5 can damage nerves that control the diaphragm-the main breathing muscle. Without help, these people can’t breathe on their own. Assisted cough devices, chest percussion, and incentive spirometry help clear lungs and prevent pneumonia. The FDA-approved implantable diaphragm pacemaker can reduce ventilator dependence by 74% in these cases.
Is spinal cord injury rehab covered by insurance?
Medicare and most private insurers cover inpatient rehab if you meet criteria (like needing 3 hours of therapy daily). But they often don’t cover everything. Wheelchairs, seating systems, FES bikes, and exoskeletons may require large out-of-pocket payments. Medicare covers 80% of wheelchair costs after your deductible, leaving $1,200-$3,500 for specialized equipment. Many people delay or skip needed devices because of cost.
How do you prevent pressure sores after a spinal cord injury?
Pressure sores happen because you can’t feel or move. Prevention starts with a proper wheelchair cushion-custom-molded, pressure-relieving. You must shift your weight every 15-30 minutes. Skin checks twice daily are essential. Use a mirror to inspect areas you can’t see. Keep skin clean and dry. Avoid sitting on hard surfaces. Even a 10-minute shift in position can prevent a serious sore.
What’s the biggest mistake people make in SCI rehab?
Waiting too long to start. Many think they need to wait until they’re “ready.” But rehab begins the moment you’re stable. Another big mistake is skipping peer support. Talking to someone who’s been through it gives you hope, practical tips, and accountability. Also, many stop exercises after a few months because they don’t see quick results. Progress is slow, but it’s real if you keep going.




Comments (10)
Shannon Hale
18 Nov 2025
This post is basically a textbook with a pulse. I’ve seen too many families waste months waiting for ‘the right time’ to start rehab-bullshit. The moment they stabilize? That’s when the real fight begins. If you’re not doing passive ROM within 72 hours, you’re already losing ground. And don’t get me started on how insurance lets people down with seating systems. $3,500 out of pocket? For a cushion? That’s not healthcare-it’s extortion.
And don’t even mention ‘miracle cures.’ If you’re still clinging to stem cell hype from 2015, you’re not helping anyone. Real progress is in FES bikes, diaphragm pacemakers, and peer mentors-not Instagram influencers with ‘spinal cord recovery secrets.’
Holli Yancey
20 Nov 2025
I appreciate how grounded this is. So many articles make SCI sound like a battle you can win with grit alone. But the truth is, it’s about systems-access, support, affordability. I’ve watched my cousin go through this, and the thing that helped most wasn’t the wheelchair or the therapy-it was the woman who’d been in a similar chair for 12 years, showing up every Tuesday just to say, ‘I know how hard today was.’
That’s the real tech. Not the $100k exoskeleton. Just someone who gets it.
Jessica Healey
20 Nov 2025
ok but like… why is everyone acting like exoskeletons are the future?? i mean sure they look cool on tiktok but one session = 45 mins of pure agony and two therapists holding you up like a baby? no thanks. i’d rather have a fes bike that i can use while watching netflix in my pajamas. also why is no one talking about how the pain from spasticity is just… always there? like, no one ever says ‘hey, your legs are randomly locking up and it feels like your bones are being crushed by invisible hands’
also who pays for this stuff??
Levi Hobbs
21 Nov 2025
Thank you for including the stats-especially the 59% incomplete recovery rate. Too many people assume ‘incomplete’ means ‘almost fixed.’ It doesn’t. It means ‘some signals get through,’ and that’s enough to rebuild independence, not restore normalcy. Also, the 68% dropout rate on home exercises? That’s heartbreaking. It’s not laziness. It’s isolation. No one sees you doing your 30 reps. No one claps. No one says, ‘You’re still here-that’s victory.’
Peer mentors aren’t a luxury. They’re the missing link in every rehab plan. And yes, the cost of seating systems is a national scandal.
henry mariono
22 Nov 2025
I’m not a medical professional, but I’ve worked with a few SCI patients over the years. The thing I noticed most? The ones who thrived didn’t focus on walking. They focused on control. Dressing themselves. Managing their bladder without help. Transferring from bed to chair without screaming. Those are the wins that last. The rest? The exoskeletons, the FES bikes-they’re tools. Not goals.
And the diaphragm pacemaker? That’s the quiet revolution no one talks about. It’s not flashy, but it gives people back their breath. That’s everything.
Sridhar Suvarna
22 Nov 2025
Respect for this detailed and compassionate overview. In India, access to such care is nearly nonexistent outside major cities. Many families rely on traditional healing or delay treatment due to cost. The idea of a custom cushion costing $3,500 is unimaginable. Yet the principles here-early rehab, peer support, functional independence-are universal.
We need global advocacy. Not just for tech, but for equity. A man in Delhi deserves the same chance at dignity as a man in Chicago. The science is here. The will must follow.
Joseph Peel
23 Nov 2025
One thing this post omits: the psychological toll of being treated as a ‘case study’ instead of a person. I’ve been in rehab centers where therapists treat you like a lab rat-‘Let’s test your reflexes,’ ‘Try to move your toe again,’ ‘Do you feel that?’ No one asks if you slept. No one asks if you miss dancing. No one asks if you’re angry.
Rehab isn’t just muscles and nerves. It’s identity. And too many programs treat the body like a machine that needs tuning, and forget the soul that’s still inside it.
Kelsey Robertson
24 Nov 2025
Okay, but let’s be real-how many of these ‘miracle’ devices are just glorified toys funded by venture capitalists who’ve never met someone with SCI? Exoskeletons? $100,000? For 45 minutes of standing? Meanwhile, people can’t afford basic catheters. And don’t get me started on ‘AI-personalized therapy plans’-what’s next? An algorithm telling you when to cry?
The real breakthrough? Someone who actually listens. Not a machine. Not a patent. A human who says, ‘I see you. You’re not broken. You’re adapting.’ That’s the only cure that matters.
Joseph Townsend
24 Nov 2025
Y’all are acting like this is some kind of sci-fi documentary. This is real life. I’ve seen it. I’ve lived it. The first time I had to ask my mom to wipe my ass after a bowel program? That was the day I stopped being a person and became a patient. The exoskeleton? The FES bike? The diaphragm pacemaker? They’re not magic. They’re bandaids on a bullet wound.
But here’s the truth: I still laugh. I still date. I still drive. I still cook. I still hate my damn wheelchair when it squeaks. This isn’t about walking again. It’s about refusing to let a broken spine define your whole damn life. And that? That’s the real revolution.
Shannon Hale
26 Nov 2025
Joseph Townsend just said it better than I ever could. That’s the heart of it. You don’t heal from this. You rebuild. And if you’re lucky, you rebuild with rage, humor, and a damn good power chair that doesn’t squeak. The system’s broken. But people? We’re not. We’re still here. Still fighting. Still living. And that’s more than any rehab program, any device, any insurance policy can ever give you.
Now if you’ll excuse me-I’ve got a wheelchair to fix and a pizza to eat with one hand.