Generic Substitution: What It Is, How It Saves Money, and What You Need to Know
When your pharmacist hands you a pill bottle with a different name than your doctor wrote, that’s generic substitution, the practice of replacing a brand-name drug with a chemically identical generic version approved by the FDA. Also known as therapeutic equivalence, it’s one of the biggest ways healthcare cuts costs without sacrificing safety. Most people assume all generics are the same, but not every drug can be swapped—and not every swap is automatic. The FDA uses Therapeutic Equivalence Codes (TE Codes), a rating system that tells pharmacists which generics can legally replace brand drugs to make sure you get the right medicine, not just a cheaper version. If a drug has an AB1 rating, it’s a direct substitute. If it’s an BX, it’s not approved for substitution at all.
Why does this matter? Because your insurance plan often pushes you toward generics to save money. But if your doctor wrote a brand name and the pharmacist switches it without checking the TE code, you could end up with a drug that doesn’t work the same way. Some medications—like blood thinners, thyroid pills, or seizure drugs—need to be exact. Even tiny differences in how they’re made can throw off your dose. That’s why authorized generics, the exact same drug as the brand, just sold under a different label exist. They’re rare, but when available, they’re the safest swap. Most generics, though, are made by different companies with different manufacturing processes. That’s why contamination controls, cleanroom standards, and FDA inspections are so critical.
Not all drugs even have generics. Some brand companies block them with legal tricks, patent extensions, or by refusing to release the formula. Others, like complex injectables or biologics, are too hard to copy. That’s why you might still pay full price even when a generic seems like it should exist. And if you’re on Medicare Part D, your drug’s tier level determines how much you pay—so even if a generic is available, it might not be the cheapest option unless you request a tier exception. The real power of generic substitution comes when you know how to ask for it, check your formulary, and understand what your pharmacist can and can’t change without your doctor’s okay.
Below, you’ll find real guides from people who’ve navigated this system—how to check coverage before switching plans, how to fight for lower copays, what to do when your insurance denies a generic, and why some drugs just won’t switch no matter how much you save. This isn’t theory. It’s what happens in pharmacies, clinics, and homes every day when someone tries to cut costs without risking their health.
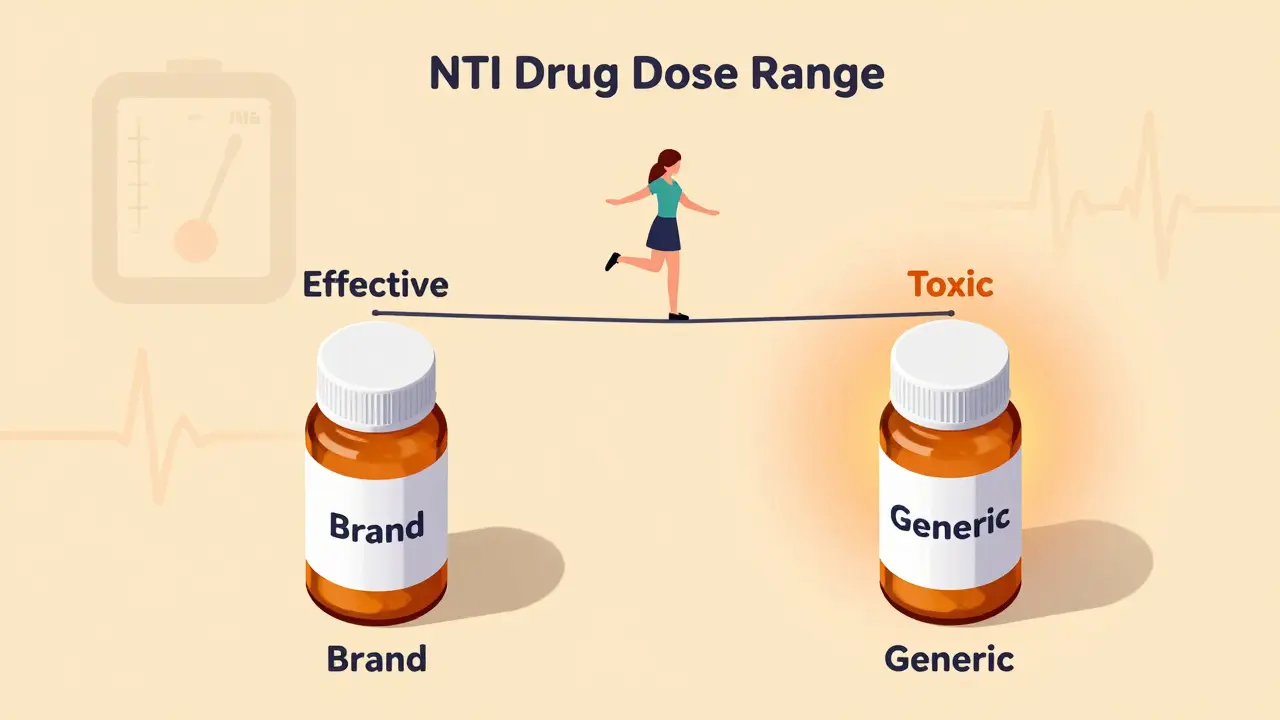
NTI drugs like warfarin and phenytoin have a tiny margin between effective and toxic doses. Generic substitutions can push patients out of this narrow range, risking serious harm - even death. Here’s why switching isn’t always safe.
Pharmacists can legally substitute generic drugs in all U.S. states, but therapeutic substitution rules vary widely. Learn how state laws shape what pharmacists can do, the documentation required, and why this matters for patient access and safety.
Pharmacists face real challenges when substituting brand-name drugs with generics-patient mistrust, unclear doctor guidance, and time constraints. Here’s what really happens behind the counter and how to make it work.