Common Pharmacist Concerns About Generic Substitution: What Really Happens Behind the Counter

Every day, pharmacists in the UK and beyond face the same quiet tension: a prescription for a brand-name drug lands on the counter, and the law says they can swap it for a cheaper generic. Sounds simple, right? But behind that routine decision lies a web of patient doubts, physician hesitation, and real clinical worries that most people never see. For pharmacists, generic substitution isn’t just about saving money-it’s about trust, timing, and sometimes, fear.
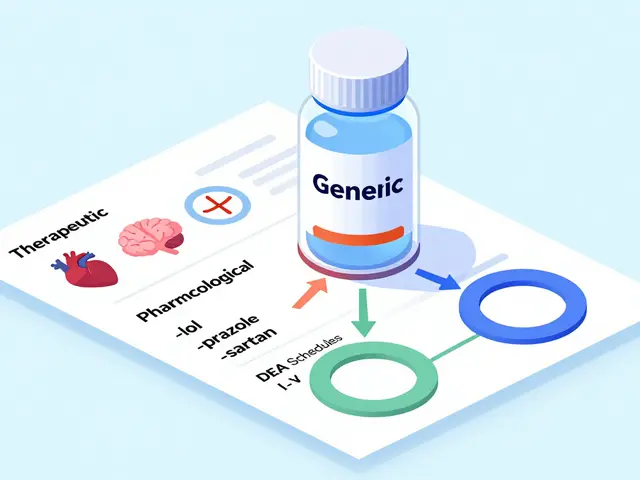
Why Pharmacists Are Asked to Substitute
Generic drugs aren’t knock-offs. They’re exact copies of brand-name medicines in active ingredient, strength, and how they’re taken. The FDA and similar agencies require them to be bioequivalent-meaning they work in the body within 80-125% of the original. That’s not a guess. It’s backed by over 2,000 human studies showing an average absorption difference of just 3.5%. In practice, this means for 9 out of 10 patients, switching to a generic does nothing to the outcome. But here’s the catch: pharmacists are the ones who have to explain this. Not doctors. Not insurance companies. Not the government. Pharmacists. And they’re often the first-and sometimes only-person a patient talks to about the switch.The Patient Who Doesn’t Believe It Works
You’d think if a pill is cheaper, people would be happy. But many aren’t. In fact, nearly half of patients worry that lower price equals lower quality. One woman in Sheffield came in for her blood pressure med. Her doctor prescribed the brand. The pharmacist offered the generic. She refused. "It’s the same thing," the pharmacist said. She replied, "But my husband’s brand comes in a blue pill. This one’s white. How can that be the same?" This isn’t rare. Studies show that changes in pill shape, color, or size-things patients notice immediately-trigger anxiety. Especially among older adults and those on multiple meds. One Australian study found that patients with dementia or mental health conditions were the most likely to refuse substitution, not because they didn’t understand, but because they’d been burned before. A bad reaction, even if unrelated, made them distrust anything new. And it’s not just about looks. Some patients were told by their doctor, "This brand is special," even if it wasn’t true. Now the pharmacist has to undo that message in five minutes while the line grows behind them.The Silent Conflict Between Doctors and Pharmacists
Doctors get it. They know generics save money. A survey showed 87% of GPs think generic substitution is economically smart. But only 70% believe it’s clinically safe. That gap matters. Take epilepsy meds. Or thyroid pills. Or warfarin. These are narrow therapeutic index (NTI) drugs. A tiny change in how much gets into the bloodstream can mean the difference between control and crisis. Pharmacists know this. They’ve seen patients who stabilized on a brand, then switched to a generic-and had a seizure, or a clot, or a fall. Was the generic to blame? Maybe not. But the timing looked bad. And that’s all it takes for a doctor to say, "Never switch this one again." The problem? The FDA says bioequivalence is enough. But doctors don’t always trust the data. And when they don’t, they write "Do Not Substitute" on the script. That’s fine-unless they don’t tell the pharmacist. Or they write it in tiny handwriting. Or they forget to update the electronic system. Now the pharmacist has to guess. And if they guess wrong, someone gets hurt.
The Time Crunch Nobody Talks About
Pharmacists aren’t just dispensing pills. They’re counselors, educators, and sometimes, therapists. A 2015 U.S. survey found that 64% of patients had never heard from their doctor that generics were an option. So when the pharmacist offers one, they’re not just handing over a pill-they’re delivering a lecture. "This is the same medicine. It’s cheaper. It’s FDA-approved. You can ask your doctor if you want. But you don’t have to take it." That’s the script. And it takes 90 seconds. But in a busy pharmacy, that’s 90 seconds you don’t have. And if the patient says, "I want to talk to my doctor," now you’ve got a phone call to make, a note to write, and a refill delay that could cost the patient their job or their health. Worse? Only 38% of patients are told they can refuse the substitution. That’s not just a gap-it’s a legal risk. Pharmacists are supposed to inform patients of their right to decline. But in the rush, it’s easy to forget. And if a patient later claims they weren’t told, the pharmacist is on the hook.The Real Cost of a Generic Switch
It’s easy to say generics save 21% on drug costs. But what’s the real cost to the system? When a patient refuses a generic, the pharmacy has to reorder the brand. That’s extra shipping, extra paperwork, extra inventory cost. When a patient switches and then has a bad reaction, even if it’s unrelated, the doctor may stop prescribing generics altogether. That means higher costs for everyone. And then there’s adherence. If a patient doesn’t understand why they’re getting a different pill, they might stop taking it. Or take it at the wrong time. Or think it’s not working. A review in the GABI Journal found that poor understanding of substitution led to increased medication errors and higher hospital admissions. That’s not just a clinical issue-it’s a financial one. A single hospital admission can cost 20 times more than a year’s supply of generics.
What Works: Real Solutions from the Front Lines
So what do good pharmacists do differently? They don’t wait for the patient to ask. They lead. They say, "I see you’re on this brand. We can switch to a generic that’s identical in active ingredient and works the same way. It’s about £15 cheaper per month. Some people worry about the color change-that’s just the filler. The medicine inside is the same. You’re welcome to keep the brand if you prefer. But if you’re okay with the switch, I’ll make sure your doctor knows we did it." They keep a list of drugs where substitution is risky-NTI meds, anti-seizure drugs, blood thinners-and flag them before they even reach the counter. They use the FDA’s 3.5% absorption difference stat. Not to sound smart. But to calm nerves. They also push back gently on doctors. If a doctor writes "Do Not Substitute" on every script, a good pharmacist will ask why. Sometimes, it’s habit. Sometimes, it’s outdated info. Sometimes, it’s fear. And if the pharmacist can show data-"Here’s the study on this drug’s bioequivalence"-they can change minds.The Bigger Picture: Who’s Really in Charge?
The truth? No one is really in charge. The law says pharmacists can substitute. The science says it’s safe. The patients are confused. The doctors are unsure. The system is designed to save money-but it’s not designed to help people understand. Pharmacists are stuck in the middle. They’re the ones who get blamed if something goes wrong. But they’re rarely given the time, training, or authority to fix the root problem: poor communication. The answer isn’t more rules. It’s more conversations. More trust. More clarity. And it starts with pharmacists having five minutes with every patient-not to sell a drug, but to explain why it’s safe. Because in the end, a generic pill doesn’t need to look like the brand. But the patient needs to feel like they’re still getting the same care.Are generic drugs really as effective as brand-name drugs?
Yes, for the vast majority of medications. Generic drugs must meet the same strict standards as brand-name drugs. They contain the same active ingredient, in the same strength, and work the same way in the body. The FDA requires them to be bioequivalent-meaning they’re absorbed at a rate and extent that falls within 80-125% of the brand. Over 2,000 studies confirm this. For most people, switching makes no difference in how well the drug works.
Why do some patients refuse generic substitutions?
Many patients associate pill appearance-color, shape, size-with effectiveness. If their brand was blue and the generic is white, they think it’s different. Others fear foreign manufacturers or believe lower price means lower quality. Patients with chronic conditions, dementia, or mental health issues are especially likely to resist change. Past negative experiences, even if unrelated to the drug, can fuel mistrust. And if their doctor never mentioned generics, they assume the brand is "better."
Can pharmacists refuse to substitute a drug?
Pharmacists can’t refuse substitution if the prescription allows it and the drug is approved for swap. But they can and should refuse if the drug is on a list of high-risk medications like anti-seizure drugs, blood thinners, or thyroid meds-where small differences in absorption matter. Also, if the patient refuses, the pharmacist must honor that. The law gives patients the right to decline a generic, even if the pharmacist recommends it.
What should pharmacists do when a patient is worried about switching?
Don’t just say "it’s the same." Explain: "This pill has the same active ingredient as your brand, just made by a different company. The FDA checks it to make sure it works the same way. The only difference is the color or shape-that’s just the filler, not the medicine. It’s cheaper, but just as safe." Use the 3.5% absorption difference stat to show it’s not a gamble. Offer to call the doctor if they’re unsure. And always remind them they can keep the brand if they prefer.
Are there drugs where generic substitution is risky?
Yes. Drugs with a narrow therapeutic index (NTI) are the main concern. These include warfarin, levothyroxine, phenytoin, and some epilepsy meds. Even small changes in blood levels can lead to serious side effects. While generics are still approved as bioequivalent, many pharmacists and doctors prefer to keep stable patients on the same version-brand or generic-to avoid any risk. Pharmacists should flag these drugs and consult with the prescriber if substitution is suggested.
Why don’t doctors talk to patients about generics?
Many doctors assume patients already know. Others are worried about causing confusion. Some still believe brand-name drugs are superior, even without evidence. A U.S. study found 55% of patients never discussed cost with their doctor. That leaves pharmacists to fill the gap-often without enough time or support. When doctors do mention generics, patient acceptance jumps by 30% or more.
What’s the biggest barrier to successful generic substitution?
The biggest barrier isn’t science or cost-it’s communication. Patients don’t understand why they’re getting a different pill. Doctors don’t consistently support the switch. Pharmacists are left to explain it all in a few minutes. Without clear, consistent messaging from the whole healthcare team, substitution becomes a source of anxiety, not savings.



Comments (12)
Saket Modi
2 Dec 2025
lol another pharmacist sob story. 🤡
Girish Padia
4 Dec 2025
People don't get it. Generic isn't cheap because it's bad. It's cheap because the patent ran out. Same chemistry. Same results. But no one wants to believe the system isn't out to screw them.
Chris Wallace
5 Dec 2025
I’ve seen this play out in my mom’s pharmacy visits. She’s 72, on six meds, and every time the pill changes color, she panics. Not because she’s irrational-because she’s been burned before. One time, they switched her thyroid med and she had a panic attack for three days. Turned out it wasn’t the drug, but the pharmacy didn’t explain anything. Just handed her a new pill. That’s not healthcare. That’s logistics with a white coat.
william tao
7 Dec 2025
It is a matter of profound concern that pharmacists, who are not trained physicians, are being entrusted with the de facto authority to substitute life-sustaining pharmaceuticals based on cost-efficiency metrics alone. This represents a systemic abdication of clinical responsibility by the medical establishment. The FDA’s 80-125% bioequivalence window is not a therapeutic guarantee-it is a statistical loophole exploited by corporate interests. When a patient’s seizure threshold is compromised by a 12% absorption variance, who bears moral culpability? Not the pharmacist. Not the insurer. Always the patient.
Sandi Allen
8 Dec 2025
They’re lying. Always lying. The FDA? Controlled by Big Pharma. The generics? Made in India and China with dirty labs. My cousin’s uncle’s neighbor took a generic blood thinner and ended up in a coma. They never told her it wasn’t the same! And now they want us to trust pills that look like candy? No. No. No. This is how they control us. Lower prices? More like lower standards. Wake up.
John Webber
8 Dec 2025
why do ppl think cheaper = bad? its the same stuff!! i got my blood pressure med generic and saved 40 bucks a month. my doc said its fine. my pills are white now but i dont feel any different. stop overthinking it. also why do pharmacists have to be therapists? just give me the pill.
Shubham Pandey
9 Dec 2025
Generic works. Stop making it a thing.
Elizabeth Farrell
10 Dec 2025
I just want to say how much I appreciate pharmacists doing the emotional labor no one else will. You’re not just handing out pills-you’re holding space for people who are scared, confused, and overwhelmed. The fact that you’re trying to explain bioequivalence while juggling 12 other patients? That’s quiet heroism. And to those saying it’s ‘just a pill’-you’ve never been the person who’s had to relearn how to take your meds after a switch. Be gentle. Listen. And thank you-for showing up even when the system doesn’t.
Sheryl Lynn
10 Dec 2025
The real tragedy isn’t the substitution-it’s the commodification of pharmacology into a transactional, aesthetic experience. The pill’s chromatic variance is not merely a filler discrepancy; it is a semiotic rupture in the patient’s therapeutic narrative. The color, the shape, the imprint-these are not arbitrary. They are talismans of continuity, of identity, of psychological anchoring. To dismiss this as ‘irrational’ is to misunderstand the phenomenology of adherence. We are not dispensing molecules-we are restoring existential stability.
Paul Santos
12 Dec 2025
Classic case of systemic misalignment, no? 🤔 We’ve got a healthcare model that incentivizes cost-cutting but expects frontline workers to shoulder the cognitive burden of patient education. Meanwhile, the doctor who wrote ‘Do Not Substitute’ in pencil on a 20-year-old script is still getting paid £120/hr for a 5-minute consult. Meanwhile, the pharmacist is doing 200 consults a day with zero time to breathe. It’s not a crisis of trust-it’s a crisis of design. And no, the 3.5% stat won’t fix that. 😅
Eddy Kimani
12 Dec 2025
Interesting data on NTI drugs. Have you seen the 2023 meta-analysis from the Journal of Clinical Pharmacology on levothyroxine bioequivalence across 14 manufacturers? The intra-individual variability in absorption was higher between different generic batches than between brand and generic. That’s the real issue-not whether generics work, but whether we’re treating them as interchangeable commodities when they’re not. We need batch tracking and patient-specific logs. Not just ‘it’s the same’.
Chelsea Moore
12 Dec 2025
HOW DARE THEY?!?! The system is OUT TO GET US!!! They switch your pills without warning, and then you get dizzy, and you think it’s you-BUT IT’S THE GENERIC!!! And no one listens!! I had a seizure after switching!!! And now they say it’s ‘psychosomatic’??? I KNOW WHAT HAPPENED!!! THEY’RE HIDING THE TRUTH!!! I’M NOT CRAZY-I’M A VICTIM!!!