Teaching Children About Medication Safety at Home and School

Every year, 50,000 children under five end up in emergency rooms because they accidentally swallowed medicine they shouldn’t have. Many of these cases happen at home - a child grabs a bottle left on a nightstand, finds a brightly colored liquid in a purse, or thinks a pill looks like candy. At school, the risk isn’t much lower. Without clear rules and trained staff, medications can be mixed up, given at the wrong time, or taken by the wrong child. The truth is, kids aren’t just curious - they’re watching. And if they see an adult take medicine without thinking, they’ll copy it. Teaching children about medication safety isn’t about scaring them. It’s about giving them clear, simple rules they can live by - at home, at school, and everywhere in between.
Why Kids Mistake Medicine for Candy
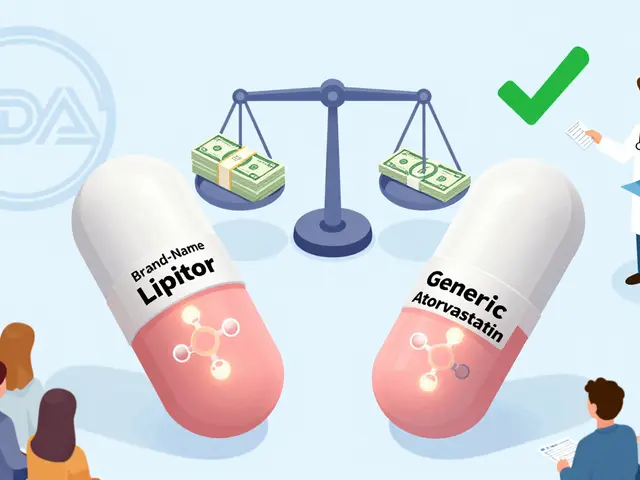
It’s not that children are being reckless. It’s that medicine is often designed to taste good. Liquid antibiotics come in cherry, grape, or bubblegum flavors. Chewable tablets look like gummy bears. Even vitamins can be shaped like animals or coated in sugar. The FDA warns that calling medicine "candy" - even jokingly - increases the chance a child will swallow it by 220%. That’s not a guess. It’s based on data from over 1,200 poisoning cases. When a parent says, "This will help you feel better, just like candy," the child hears: "This is something I can eat whenever I want." The fix is simple: never say "candy" around medicine. Say it plainly: "This is medicine. Medicine is not candy. Only adults can give it to you." Say it every time. Even if it feels repetitive. Repetition builds safety. And when a child sees you take your own pills, don’t do it in front of kids under four. A 2021 FDA study found that 78% of toddlers under three copied the behavior within a minute. If you need to take your medicine, wait until the child is out of the room.What Kids Should Know at Each Age
Children learn differently at every stage. There’s no one-size-fits-all lesson. Here’s what works, based on guidelines from the FDA and pediatric experts:- Ages 3-4: Teach them to give any pill or bottle they find to a grown-up. No tasting. No playing. Just hand it over. Use role-play: "What if you find this on the floor?" Practice with empty bottles or toy medicine kits. Reward them for telling you - don’t punish them for finding it.
- Ages 5-6: They can start to recognize medicine bottles. Let them put their name on their own medicine with a sticker. Teach them that medicine must always be kept up and away - not on the counter, not in a purse, not under the bed. Ask them: "Where do we keep medicine?" If they say "on the table," you know there’s work to do.
- Ages 7-8: They can help read labels. Show them the name on the bottle. Compare it to the doctor’s instructions. Teach them to ask: "Is this mine?" and "When do I take this?" They should also learn their own weight - even roughly - because dosing depends on it. A child who weighs 40 pounds needs less than one who weighs 70 pounds. Using a kitchen spoon? That’s risky. A 2022 study found household spoons cause 40-98% dosing errors. Use the little plastic syringe that comes with the medicine. Pharmacies give them out for free.
How Schools Can Help - And Where They Fall Short
Schools are a second home for many kids. That’s why medication safety needs to be part of the school day - not an afterthought. Programs like Generation Rx’s "Medication Safety Patrol" turn lessons into games. Kids become "safety agents" who spot unsafe medicine storage, practice what to do if they find a pill, and learn to tell a teacher if someone else is taking medicine without permission. But not all schools can do this. Only 39% of U.S. schools have a full-time nurse. In rural areas, that number drops to 32%. That means teachers, aides, and even lunch staff are often asked to give medicine without training. Head Start programs have strict rules: all staff must complete 8 hours of initial training and 2 hours every year. They learn how to check labels, document every dose, recognize allergic reactions, and dispose of unused medicine safely. But most public schools don’t have that level of support. The result? Medication errors happen most often during transitions - when a child moves between classrooms, when a grandparent picks them up, or when a new caregiver comes in. One school district in Ohio cut medication incidents by 34% in two years by training every staff member and using the same checklist every time. That’s the kind of consistency kids need.
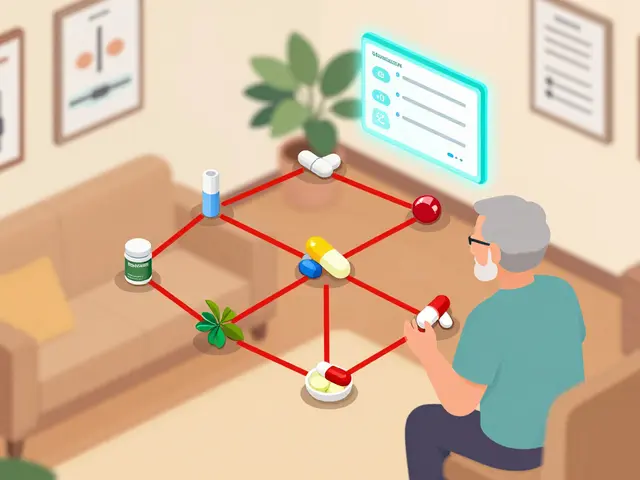
Storage Is the First Line of Defense
No lesson will work if medicine is within reach. The CDC says 67% of poisonings in kids aged 1-4 could be prevented with proper storage. That means:- Keep all medicine - even vitamins and cough syrup - in a locked cabinet, not a drawer.
- Use a lock box that meets ASTM F2057-22 safety standards. These are tested to resist kids who try to open them.
- Never leave medicine on nightstands, kitchen counters, or in purses, backpacks, or suitcases.
- Grandparents and visitors? They’re the biggest risk. A CDC survey found 79% of grandparents don’t follow safe storage rules when kids visit. Keep a separate locked box at their house if your child spends time there.
What to Do If a Child Swallows Medicine
Even with all the rules, accidents happen. That’s why every home and school must have the Poison Help number: 800-222-1222. Program it into every phone. Save it in your contacts as "Poison Help." Don’t wait to see if the child looks sick. Don’t try to make them throw up. Don’t call 911 first unless they’re unconscious or having trouble breathing. Call Poison Help. They’ll tell you exactly what to do - and they’re available 24/7. The National Poison Control Center says 91% of calls about kids swallowing medicine come within one hour of the incident. Speed saves lives. Keep the number posted next to every phone. Teach your child to dial it if they’re alone and feel strange after touching medicine.
What’s Missing: Teaching Teens
Most programs stop at age 10. That’s a problem. Prescription misuse peaks at age 16. Teens are taking pills from their parents’ medicine cabinets - not because they’re curious, but because they think it’s harmless. They see adults taking medicine every day. They don’t realize a painkiller meant for a backache can be dangerous when taken without a doctor’s order. Experts say we’re failing teens by not talking to them about medication risks. The CDC is starting to fix this in 2024 by expanding its PROTECT Initiative to include middle and high school programs. But schools need help. We need lessons that explain: why pills are powerful, how they affect the brain, and what addiction looks like. We need to treat medication safety like sex ed or drug prevention - not as something just for little kids.Tools That Actually Work
You don’t need fancy gadgets. But you do need the right tools:- Oral syringes: For liquid medicine. No spoons. No cups. Use the one that came with the prescription.
- Medication lock boxes: Look for ASTM F2057-22 certification. They cost under $20.
- Medication logs: A notebook or app where you write down what was given, when, and by whom. Schools need these. So do families.
- Free resources: Generation Rx offers printable games and videos for classrooms. The FDA has an interactive site called "Med Safety for Kids" with games for ages 4-10.
Final Thought: Safety Is a Habit, Not a Lesson
You can’t teach medication safety in one talk. It’s not a lesson. It’s a habit. It’s what you say every time you open a bottle. It’s where you put the medicine after you use it. It’s how you answer when your child asks, "Can I have this?" It’s what your school does when a child brings in an inhaler or insulin. The goal isn’t to make kids afraid of medicine. It’s to make them respectful. To make them curious, but cautious. To make them the kind of kids who say, "I’ll get an adult," instead of "I’ll try it." And that’s the kind of safety that lasts.At what age should children start learning about medication safety?
Children can start learning as early as age 3. At this age, they can understand simple rules like "give any pill you find to an adult" and "medicine is not candy." The key is using age-appropriate language and role-playing. By age 5, they can begin recognizing medicine bottles and understanding that medicine must be kept out of reach. Early lessons build a foundation for more complex understanding as they grow.
Can child-resistant caps alone prevent children from accessing medicine?
No. Child-resistant caps are not enough. Studies show that toddlers can open many of these caps in under a minute. The CDC found that only 29% of parents who rely solely on child-resistant caps store medicine safely. In contrast, 86% of parents who use a locked storage box keep medicine out of reach. A locked box that meets ASTM F2057-22 safety standards is the most effective way to prevent accidental access.
Why is it dangerous to take medicine in front of young children?
Children under 4 learn by imitation. A 2021 FDA study found that 78% of toddlers aged 2-3 copied the behavior of an adult taking medicine within 60 seconds. Even if you think they’re not paying attention, they are. Taking medicine in front of them teaches them that it’s normal to handle pills and liquids without permission. Always wait until they’re out of the room to take your own medication.
What should I do if my child swallows medicine by accident?
Call Poison Help immediately at 800-222-1222. Don’t wait for symptoms to appear. Don’t try to make your child vomit. Don’t give them milk or food unless instructed. Poison Help operators are trained to guide you through exactly what to do based on the medicine swallowed, the amount, and your child’s age and weight. Keep this number saved in every phone in your home and teach older children how to dial it.
Are there free resources available to teach medication safety in schools?
Yes. Generation Rx offers a free Elementary Toolkit with 12 classroom activities, 8 instructional videos, and 15 printable worksheets for grades K-5. The FDA also provides a free digital platform called "Med Safety for Kids," featuring interactive games for children aged 4-10. Many pharmacies also give out free oral syringes and educational brochures. Schools with limited budgets can use these resources to build a full safety program without spending money.
Why is using a kitchen spoon to measure medicine dangerous?
Kitchen spoons vary in size and aren’t designed for accurate dosing. A 2022 study found that using household spoons leads to dosing errors between 40% and 98%. That means a child could get too little medicine - and it won’t work - or too much - and it could be harmful. Always use the oral syringe or dosing cup that comes with the prescription. These are marked with exact measurements and are designed for children’s safety.




Comments (10)
Lana Kabulova
23 Jan 2026
I can't believe we still have to say this: medicine is NOT candy. My 3-year-old saw me take a pill last week and asked if he could have one 'for the taste.' I nearly had a heart attack. Now I take meds in the bathroom with the door locked. No more excuses.
Margaret Khaemba
24 Jan 2026
My mom used to say 'this is like candy' to get my sister to take antibiotics. She ended up in the ER at age 2. I don't say 'candy' anymore. Ever. Even when I'm tired. Even when I'm joking. I say 'medicine' like it's a sacred word. And my kid knows it. No more accidents on my watch.
Malik Ronquillo
26 Jan 2026
Wow. So we're just gonna blame parents and grandparents now? What about the pharmaceutical companies that make pills look like Skittles? And why are we teaching kids to be scared of medicine instead of teaching them how to be responsible? This feels like over-parenting with a side of fearmongering.
Brenda King
28 Jan 2026
I teach kindergarten and we do a weekly 'medicine safety check' with toy bottles and stickers. Kids love it. They call themselves 'Medicine Guardians.' We even have a poster with the poison number. It's simple. It works. And no one has had an accident in 3 years. Small habits, big results. 🙌
Keith Helm
29 Jan 2026
The CDC data is clear. Locked storage reduces incidents by 86%. Child-resistant caps are insufficient. Schools without nurses are failing children. These are not opinions. They are facts.
Alec Amiri
29 Jan 2026
Let's be real - most parents don't even know how to use a syringe. I've seen people pour syrup into a soda cap. And now we're gonna teach 4-year-olds about ASTM standards? Come on. Just keep the meds locked up and stop acting like every kid is a future drug dealer.
Rob Sims
29 Jan 2026
Oh great. Another guilt-trip article. So now I'm a bad parent because I leave my allergy pills on the nightstand? My kid’s 5. He’s never touched them. And you want me to lock them up like they’re heroin? I’ll wait until the government starts giving me a medal for not letting my kid eat Tylenol.
arun mehta
31 Jan 2026
In India, many families keep medicines in open shelves. But when we started using small lock boxes from local pharmacies - even the ones under ₹500 - accidents dropped dramatically. My neighbor’s grandson found his grandfather’s diabetes pills last year. He didn’t swallow them. He brought them to his mom. Because he was taught: 'If you see medicine, give it to grown-up.' Simple. Powerful. 🙏
Patrick Roth
1 Feb 2026
You're ignoring the real issue: kids are smart. If you treat medicine like a forbidden fruit, they'll sneak it. Better to teach them how to read labels, understand dosage, and respect pharmacology - like you teach them to cross the street. Fear doesn't teach responsibility. Knowledge does.
Kenji Gaerlan
3 Feb 2026
my kid found my advil once. i yelled. he cried. now he just hides stuff in his toy box. maybe we should just stop giving kids medicine altogether?