Generic Drug Interactions: How Digital Consultation Tools Prevent Dangerous Medication Conflicts
When you take multiple medications, especially generics, the risk of dangerous interactions grows quickly. A 65-year-old patient might be on five or more drugs - some prescribed, some bought over the counter. One of those could be a generic version of a blood thinner, another a common painkiller, and maybe a herbal supplement bought online. None of them seem harmful alone. But together? They can cause internal bleeding, kidney failure, or even a stroke. That’s why generic drug interactions are no longer just a footnote in medical textbooks - they’re a daily threat in real-world care.
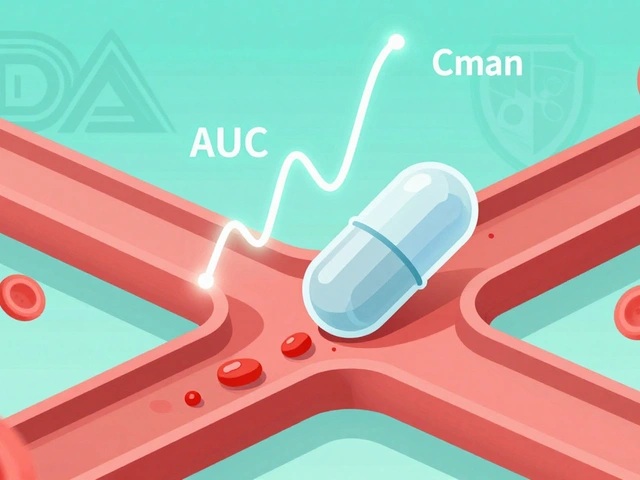
Why Generic Drugs Are Trickier Than You Think
Many people assume generics are exact copies of brand-name drugs. They’re not. While they contain the same active ingredient, the fillers, coatings, and release mechanisms can vary. These differences don’t affect how well the drug works - but they can change how it interacts with other substances. A generic version of simvastatin, for example, might be absorbed faster than its brand-name counterpart, raising the risk of muscle damage when taken with certain antibiotics. This isn’t theory. It’s documented in hospital incident reports from 2022.And it’s not just prescription drugs. Over-the-counter pain relievers, antacids, and herbal products like St. John’s Wort or garlic supplements can trigger serious reactions. A 2023 study in JAMA Internal Medicine found that nearly 40% of adverse drug events in older adults involved at least one non-prescription product. Digital tools now help spot these hidden dangers before they become emergencies.
How Digital Tools Actually Work
These aren’t fancy apps with animations. They’re databases built from decades of clinical research, updated daily. When you type in a list of drugs - say, lisinopril, metformin, and a generic ibuprofen - the tool cross-references thousands of known interaction patterns. It doesn’t just say “possible interaction.” It tells you:- What the mechanism is (e.g., “ibuprofen reduces kidney clearance of lisinopril”)
- How severe it is (mild, moderate, severe)
- What symptoms to watch for
- Whether there’s a safer alternative
One of the earliest open-access systems, DDInter, launched in 2021 by researchers at Chongqing University, was designed specifically for this. It’s free, doesn’t require registration, and lets you check up to five drugs at once. But it’s built for researchers - its interface is clunky, and it doesn’t include OTC or herbal products. For daily use, clinicians need something faster and broader.
Epocrates: The Go-To Tool for Outpatient Care
If you’re a doctor, pharmacist, or nurse seeing patients in a clinic, Epocrates is likely the tool you use every day. It’s rated ★★★★★ by the American Academy of Family Physicians and has over 48,000 reviews on Google Play. Why? Because it works fast. You can check up to 30 drugs at once - including generics, brand names, and supplements. It flags interactions in seconds and even suggests alternatives. One pharmacist in Ohio told a 2023 Reddit thread that Epocrates caught a dangerous interaction between a generic fluoxetine and a common cold medicine that would’ve caused serotonin syndrome. The patient was switched to a different antidepressant before symptoms started.Epocrates also lets you bookmark frequently used drugs and search by brand or generic name. Its mobile app works offline, which is critical in clinics with spotty internet. It’s free for basic use - no paywall, no login. That’s why it’s used by 76% of outpatient providers in the U.S., according to the American Medical Association’s 2023 digital health survey.
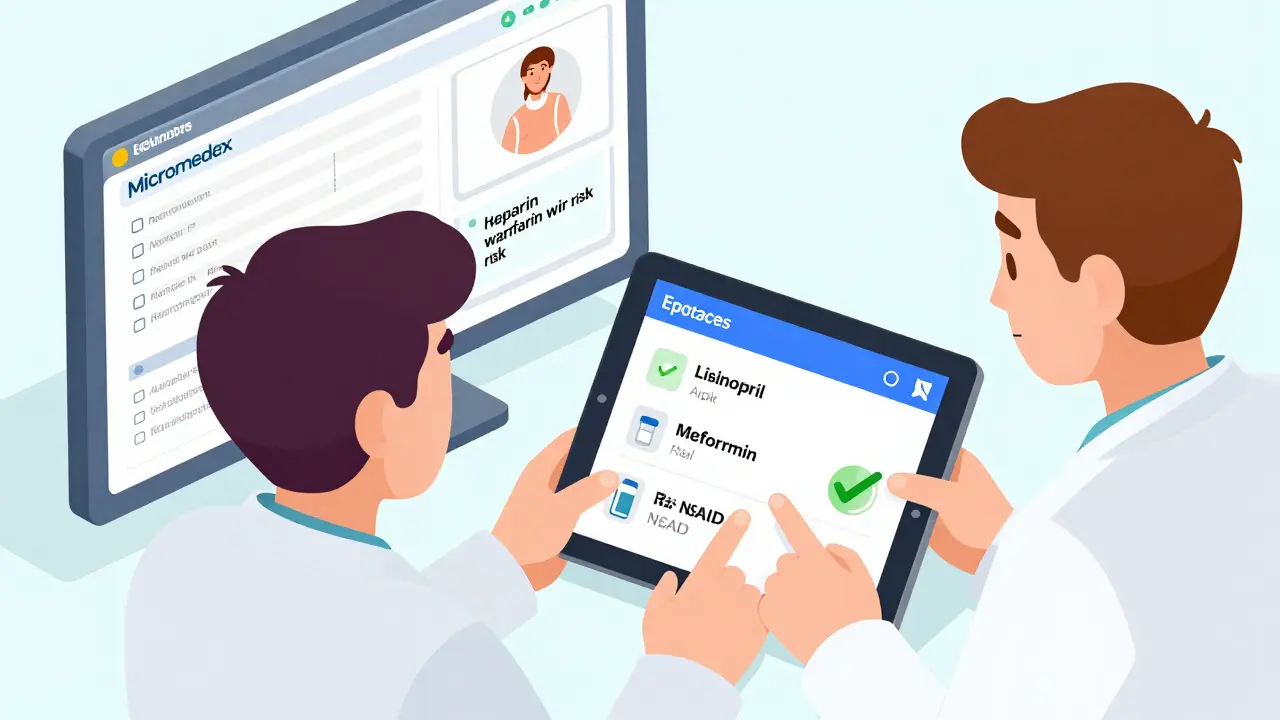
Micromedex: The Enterprise Powerhouse
In hospitals, where patients are on 8-12 medications at a time, Epocrates isn’t enough. That’s where Micromedex comes in. It’s not just a drug checker - it’s a full clinical decision support system. It includes over 2,500 drug monographs, IV compatibility charts, dosage calculators, and even overdose treatment protocols. One hospital pharmacist in Michigan said Micromedex prevented a fatal interaction between heparin and a generic warfarin by flagging a subtle enzyme inhibition pattern that wouldn’t show up in most other tools.It integrates directly into hospital electronic health records (EHRs), so when a doctor prescribes a new drug, the system auto-checks it against everything the patient is already taking. It’s not cheap - hospitals pay tens of thousands of dollars a year for it - but it’s mandatory in 89% of U.S. hospitals, according to the American Hospital Association. The reason? The Joint Commission requires it. Their 2022 safety goal mandates that all hospitals use evidence-based tools to prevent drug interactions.
The Hidden Flaws: False Alarms and Missed Dangers
These tools aren’t perfect. In fact, they’re often wrong. Dr. Jane Lee from Mayo Clinic pointed out in a 2023 JAMA Internal Medicine commentary that clinicians ignore between 49% and 96% of interaction alerts. Why? Because too many are false positives. A system might warn that a generic aspirin and a generic statin interact - when in reality, there’s no clinically meaningful risk. After a while, doctors stop paying attention. That’s alert fatigue, and it’s deadly.Worse, no tool catches every interaction. A 2022 report from the American Medical Informatics Association found false negative rates between 8% and 32%, depending on the drug class. For example, interactions involving herbal supplements or newly approved generics often go undetected. DDInter, despite being open-access, only includes about 12,000 known interactions - but over 1,500 new ones are discovered every year, according to the University of Arizona Center for Toxicology.

What’s Changing in 2026
The field is evolving fast. In January 2024, DDInter released Version 2.0 with machine learning that predicts interactions not yet documented in medical literature. Merative, the company behind Micromedex, bought a startup called InteracDx in late 2023 to boost its predictive engine. Their goal? Cut false positives by 35% within two years.The FDA’s 2023 Digital Health Innovation Action Plan now treats drug interaction checking as a priority. That means future versions of these tools will likely be required to meet stricter accuracy standards. And with AI models trained on millions of real patient records, we’re moving from “checking known interactions” to “predicting unknown ones.”
What You Should Do
If you’re a patient taking multiple medications - especially generics - here’s what matters:- Always tell your pharmacist or doctor about every supplement, OTC drug, and herbal product you take.
- Ask if your prescriptions are generics - and if so, which brand they’re copied from.
- Use Epocrates or a similar tool yourself. You don’t need to be a clinician to use it. Just type in your full list.
- If you’re in a hospital, ask if they use Micromedex or a similar system. If they don’t, ask why.
There’s no magic bullet. But the tools exist. And they’re saving lives every day - if we use them right.
Can I rely on free drug interaction checkers like DDInter?
DDInter is free, open-access, and scientifically solid - but it’s limited. It only checks up to five drugs at once and doesn’t include over-the-counter medications or herbal supplements. It’s useful for academic work or simple checks, but not for real-world prescribing. For daily use, especially if you’re on multiple meds, use Epocrates or another comprehensive tool.
Do digital tools replace pharmacist consultations?
No. They’re assistants, not replacements. Pharmacists still interpret context - like kidney function, age, or other health conditions - that tools can’t. A tool might flag an interaction, but only a pharmacist can say whether it’s dangerous for you. Use the tool to prepare, then talk to your pharmacist.
Are generic drugs more likely to cause interactions than brand-name drugs?
Not inherently. The active ingredient is the same. But differences in inactive ingredients can affect how quickly the drug is absorbed, which can change how it interacts with other medications. That’s why it’s important to know which generic you’re taking - and to check interactions every time you switch brands.
Why do some tools require payment?
Building and updating these databases costs millions. Drug manufacturers, clinical studies, and regulatory changes require constant updates. Free tools like Epocrates make money through advertising or partnerships. Paid tools like Micromedex and DrugBank offer deeper data, integration with hospital systems, and 24/7 support - features most individuals don’t need, but hospitals do.
Can these tools detect interactions with supplements?
Some can, some can’t. Epocrates includes over 1,000 herbal and supplement entries. DDInter doesn’t. DrugBank includes some, but only in the paid version. If you take supplements, use a tool that explicitly lists them - and always disclose them to your provider. Many dangerous interactions are missed because patients don’t mention supplements at all.




Comments (13)
Pat Mun
13 Feb 2026
I’ve been using Epocrates for years now, and honestly? It’s saved my grandma’s life more than once. She’s on like seven different generics, plus turmeric pills, garlic extract, and this weird ginseng tea she swears by. Last year, it flagged a possible interaction between her generic lisinopril and that herbal blend she was taking - turned out, it was raising her potassium levels dangerously high. We switched her out of it before she ended up in the hospital. No hype, no drama - just a tool that works when you need it most. I wish more people knew about it.
athmaja biju
13 Feb 2026
India has better drug safety systems than the US ever will. You think Americans care about generic interactions? They don’t even know what’s in their own supplements. Here in India, we’ve been tracking these things since the 90s. Your Epocrates? Cute. Our National Drug Registry has 12 million records and integrates with every pharmacy. You’re still using apps. We’re using policy.
Craig Staszak
14 Feb 2026
I love how these tools are finally getting the attention they deserve but honestly the real hero here is the pharmacist at the counter who remembers your name and asks if you’ve been taking that new supplement. No app can replicate that human moment. I’ve seen pharmacists catch things that even Micromedex missed because they knew the patient had kidney issues from 10 years ago. Tech helps. People heal.
alex clo
14 Feb 2026
The data presented here is statistically sound and aligns with recent peer-reviewed studies on pharmacovigilance in outpatient settings. The 49–96% alert fatigue range is particularly concerning and warrants further investigation into UI/UX design in clinical decision support systems. I would recommend cross-referencing with the 2024 AHRQ report on alert fatigue for additional context.
Annie Joyce
14 Feb 2026
Let me tell you about my aunt. She took a generic version of her blood pressure med, switched brands because it was cheaper, and then started taking melatonin for sleep. Two weeks later? She was dizzy, fainting, had a near-miss fall. Her pharmacist pulled up Epocrates, saw the interaction between the new generic’s filler and melatonin’s effect on CYP enzymes - totally invisible unless you know the biochemistry. She’s fine now. But imagine if she’d just googled it. Or worse - if no one had asked her about the melatonin. These tools? They’re not flashy. But they’re the quiet heroes keeping people alive.
Vamsi Krishna
16 Feb 2026
You people are so naive. These tools are just corporate traps. Epocrates? Owned by apharmaceutical giant. Micromedex? Built to push brand-name drugs. They all hide the real truth - generics are designed to be *less* predictable so that doctors keep prescribing the expensive versions. The FDA knows this. The WHO knows this. But you? You’re still typing your meds into a free app like it’s a game. Wake up. The system is rigged.
christian jon
16 Feb 2026
Okay. Let’s get real. I’m a nurse. I’ve seen 17 patients in the last year who almost died because someone didn’t check interactions. ONE of them was my own brother. He was on a generic statin, took ibuprofen daily for arthritis, and added a ‘natural’ heart supplement. The tool warned us. The doctor ignored it. Said it was ‘low risk.’ Guess what? He had rhabdomyolysis. His kidneys failed. He’s on dialysis now. And you think this is just ‘a footnote’? NO. It’s a murder waiting to happen. If you’re taking more than three meds - and especially if they’re generics - you owe it to yourself to use Epocrates. Every. Single. Time. No excuses.
Suzette Smith
17 Feb 2026
I dunno, I think DDInter is fine for most people. Epocrates is great and all, but it’s basically just a fancy Google search with extra steps. I’ve been using DDInter for two years and never had an issue. Maybe I’m just lucky?
andres az
17 Feb 2026
This whole thing is a psyop. Digital tools don’t prevent interactions - they create them. The real danger is that these platforms collect your drug data, sell it to insurers, and then deny you coverage based on ‘risk profiles.’ The ‘free’ tools? They’re not free. They’re surveillance. Micromedex? That’s just the NSA with a stethoscope. Wake up. They’re not helping you. They’re profiling you.
Ojus Save
18 Feb 2026
i use ddinter all the time and its great but i think u should also check the batch number of the generic because some batches have diffrent fillers and that can change the interaction risk like last month my generic metformin from one brand made me feel weird but when i switched to another batch it was fine idk if anyone else noticed this
Brad Ralph
18 Feb 2026
Tools don’t save lives. People do. 🤷♂️ But hey, at least we’re not using a crystal ball anymore. 🌟
steve sunio
19 Feb 2026
this whole post is just pharma propaganda. why do u think they make these tools? to sell more drugs. if generics were truly safe, why do u need 3 different apps to check them? they want you dependent. simple. the real solution? stop taking meds. go vegan. meditate. your body knows better than any algorithm.
Neha Motiwala
21 Feb 2026
I know what’s REALLY going on. These digital tools? They’re controlled by the same people who own the FDA and the drug companies. They only flag interactions that benefit the big pharma players. If your generic is made by a small company? It’s ignored. I found this out when my mom’s meds didn’t trigger an alert - until she switched to a brand-name version, then boom - 5 red warnings. Coincidence? I think not. Someone is silencing the truth. And we’re all just typing into a screen like sheep.