Medications Safe During Pregnancy: A Complete Patient List

When you're pregnant, even a simple headache or stuffy nose can feel like a crisis. You want to feel better-but you also don’t want to risk your baby’s health. The truth is, most common medications are safe during pregnancy, but not all. And the ones that are safe? They come with rules. Dosage limits. Trimester restrictions. Brand vs. generic confusion. Skip the Google search. This list is built from the latest guidelines from the American College of Obstetricians and Gynecologists (ACOG), the CDC, and top U.S. maternity hospitals, updated through 2024.
What’s Actually Safe? The Core List
Let’s cut through the noise. Here are the medications most doctors agree are safe when used correctly. These aren’t guesses. They’re backed by over 100,000 documented exposures tracked by the MotherToBaby registry.
- Allergy Relief: Cetirizine (Zyrtec) at 10mg once daily. Loratadine (Claritin) at 10mg once daily. Fexofenadine (Allegra) at 180mg once daily. All are non-drowsy and have been used safely in thousands of pregnancies.
- Cold & Congestion: Guaifenesin (Mucinex) for chest congestion-plain formula only. Dextromethorphan (Robitussin DM) up to 120mg in 24 hours. Saline nasal spray-no restrictions. Avoid multi-symptom formulas. They often hide decongestants.
- Pain Relief: Acetaminophen (Tylenol) is the gold standard. Maximum 3,000mg per day. That’s six 500mg tablets. Don’t go over. Avoid ibuprofen (Advil), naproxen (Aleve), and aspirin after 20 weeks. They can affect fetal kidney development.
- Heartburn & Indigestion: Calcium carbonate (Tums) as needed. Famotidine (Pepcid) up to 20mg twice daily. Both are well-studied and safe.
- Constipation: Polyethylene glycol (Miralax) at 17g daily. It doesn’t get absorbed into the bloodstream, so it doesn’t reach the baby.
- Nausea & Morning Sickness: Vitamin B6 (25mg) three times daily + doxylamine succinate (Unisom) 25mg up to three times daily. This combo is the active ingredient in Diclegis, the only FDA-approved medication for morning sickness.
What to Avoid-And Why
Some meds seem harmless. But they’re not. Here’s what to skip:
- NSAIDs after 20 weeks: Ibuprofen, naproxen, celecoxib. These can cause low amniotic fluid and heart problems in the baby. Even a single dose in the third trimester can be risky.
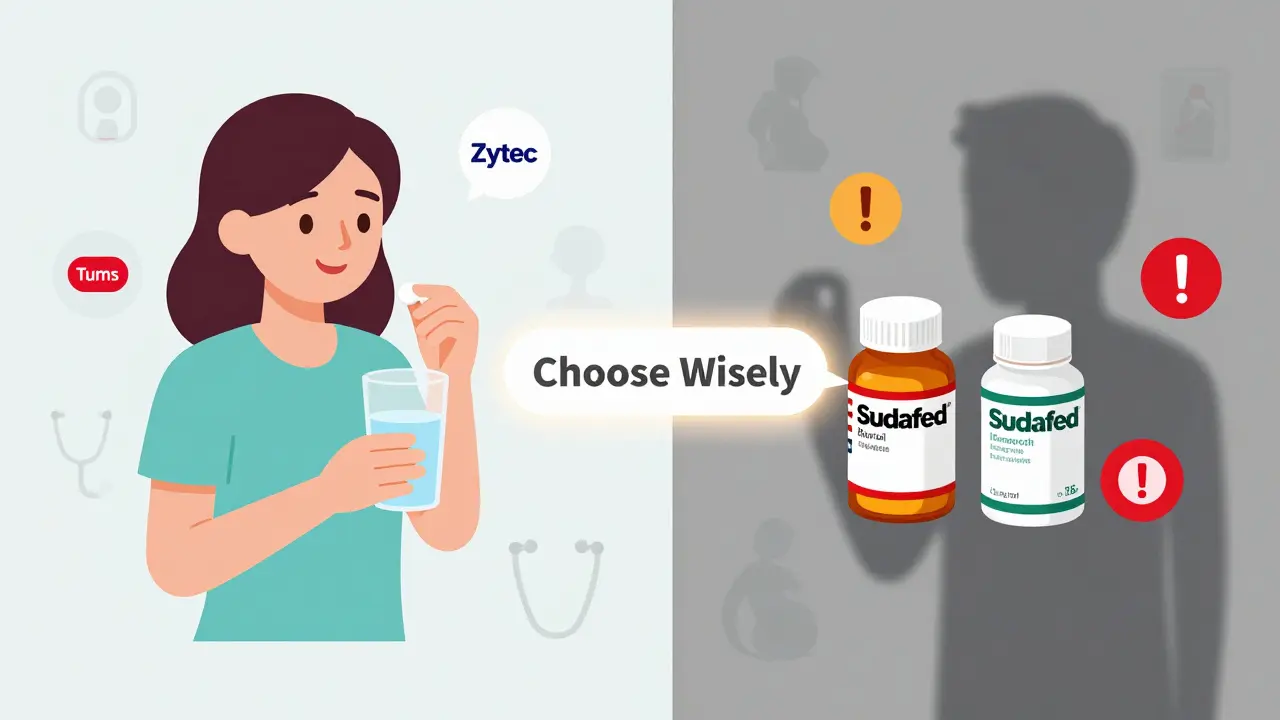
- Pseudoephedrine (Sudafed): It’s tricky. Some doctors say it’s okay after the first trimester. Others say no. The problem? It can reduce blood flow to the placenta. If you must use it, check with your provider first. In some states, you need to show ID and sign a log to buy it.
- Decongestant nasal sprays (Afrin, Neo-Synephrine): Use no more than 3 days. After that, you get rebound congestion-worse than before.
- Herbal remedies: Just because it’s “natural” doesn’t mean it’s safe. Chamomile, ginger tea in large amounts, black cohosh, and dong quai can trigger contractions or affect hormones.
- Aspirin: Except for low-dose (81mg) prescribed for preeclampsia prevention. Never take regular-strength aspirin.
Brand Names vs. Generic Ingredients
Confusion kills. You’re not buying a brand-you’re buying an ingredient. Here’s how to decode labels:
- Claritin = loratadine
- Zyrtec = cetirizine
- Allegra = fexofenadine
- Tylenol = acetaminophen
- Advil = ibuprofen
- Pepcid = famotidine
- Miralax = polyethylene glycol
Watch out for combo products. Claritin-D? That’s loratadine + pseudoephedrine. Avoid it. Robitussin? Just the plain cough syrup. Not the “Max Strength” version. That one has dextromethorphan + guaifenesin + phenylephrine. The phenylephrine? Skip it.

Dosage Matters More Than You Think
It’s not just “take one.” It’s “take one, and never more than this.”
- Acetaminophen: Max 3,000mg per day. That’s six 500mg pills. Tylenol PM? Each pill has 500mg acetaminophen + 25mg diphenhydramine. Don’t take more than six in 24 hours.
- Dextromethorphan: Max 120mg in 24 hours. That’s four 30mg doses.
- Famotidine: Max 40mg per day. Two 20mg tablets.
- Vitamin B6: Stick to 25mg per dose. Higher doses (over 200mg/day) can cause nerve damage.
Overdosing on acetaminophen is the #1 cause of acute liver failure in the U.S. It’s easy to do if you’re taking multiple products. Check every label. Even cold and flu meds often contain acetaminophen.
When to Call Your Doctor
Some symptoms need more than an OTC fix. Call your provider if:
- Your fever stays above 100.4°F for more than 24 hours
- You’re vomiting so much you can’t keep fluids down
- You have chest pain, trouble breathing, or swelling in your face or hands
- You’re taking any prescription medication-even if it’s been fine for years
- You’re unsure about a supplement, herbal tea, or “natural” remedy
Don’t assume your doctor knows what you’re taking. Many women don’t mention OTC meds because they think they’re “harmless.” But 41% of pregnant people stop necessary medications out of fear-like antidepressants-when research shows sertraline (Zoloft) and citalopram (Celexa) are among the safest options for depression during pregnancy.
The Bigger Picture: Why This Is So Confusing
Here’s the hard truth: for 73% of prescription drugs approved between 2000 and 2010, there’s still not enough data on how they affect babies. Why? Because pregnant people are rarely included in clinical trials. The FDA changed its labeling rules in 2015 to replace the old A-B-C-D-X categories with plain-language summaries. But many providers still rely on outdated charts.
And then there’s the access problem. One woman in Texas told her doctor Sudafed was okay after the first trimester. Her pharmacist refused to sell it without extra paperwork. She went three days with a bad sinus infection because no one gave her a clear answer.
Another study found that 58% of pregnant patients think herbal remedies are automatically safe. They’re not. Ginger tea is fine in small amounts. But concentrated ginger pills? That’s a different story.
What’s changing? Good things. The NIH’s PregSource project has collected over 18,700 real-world reports from pregnant people. The FDA just updated warnings for sertraline in late pregnancy. And universities are now using AI to build personalized risk models based on genetics and medical history.
But until then? Stick to the list. Use the lowest dose for the shortest time. And always talk to your provider before starting or stopping anything.
Real Stories, Real Results
One woman on BabyCenter said the B6 and Unisom combo cut her vomiting from 10 times a day to 1 or 2. Another said Zyrtec let her sleep through the night for the first time in months. But then there’s the woman who took ibuprofen for a headache at 32 weeks because “it worked better than Tylenol.” Her baby had low amniotic fluid. She had to deliver early.
There’s no one-size-fits-all. But there is a safe path. It’s not about avoiding all meds. It’s about choosing the right ones, the right way.
Is Tylenol really safe during pregnancy?
Yes, acetaminophen (Tylenol) is the safest pain reliever during pregnancy when used correctly. The maximum daily dose is 3,000mg-no more than six 500mg tablets in 24 hours. Avoid long-term daily use unless prescribed. Recent studies are looking at possible links to neurodevelopmental effects with very high or prolonged use, but the evidence isn’t conclusive. For most women, occasional use for headaches, fever, or aches is safe and recommended over NSAIDs.
Can I take Zyrtec or Claritin while pregnant?
Yes. Both cetirizine (Zyrtec) and loratadine (Claritin) are classified as low-risk and are recommended by major obstetric groups. Take the standard adult dose: 10mg once daily. Avoid the “D” versions-they contain pseudoephedrine, which should be avoided in early pregnancy. These antihistamines have been studied in over 35 years of pregnancy exposure data with no increased risk of birth defects.
Is it safe to take Mucinex while pregnant?
Plain Mucinex (guaifenesin) is considered safe for chest congestion during pregnancy. Use the standard dose: 200-400mg every 4-6 hours, not exceeding 2,400mg per day. Avoid Mucinex DM, Mucinex Fast-Max, or any multi-symptom versions-they often contain dextromethorphan, pseudoephedrine, or phenylephrine, which are not recommended. Stick to the plain formula.
What about Sudafed? Can I use it?
Pseudoephedrine (Sudafed) is controversial. Some providers say it’s okay after the first trimester. Others advise against it entirely. It can reduce blood flow to the placenta and may raise blood pressure. If you have high blood pressure, diabetes, or thyroid issues, avoid it. In some states, you need to show ID and sign a log to buy it. If you must use it, talk to your doctor first, use the lowest dose for the shortest time, and avoid it in the first trimester.
Can I take ibuprofen in early pregnancy?
It’s not recommended, even in early pregnancy. While the risk of birth defects is low before 20 weeks, ibuprofen can interfere with early fetal development, including hormone regulation. Acetaminophen is always the better choice. If you accidentally took ibuprofen once before you knew you were pregnant, don’t panic-but avoid it from now on. Always check with your provider if you’re unsure.
Are herbal teas safe during pregnancy?
Some are, some aren’t. Ginger tea in small amounts (1-2 cups daily) is generally safe and helps with nausea. Peppermint tea is okay in moderation. But avoid chamomile, licorice root, sage, and black cohosh-they can trigger contractions or affect hormones. Don’t assume “natural” means safe. Always check with your provider before drinking herbal teas regularly.
What if I’m on antidepressants?
Do not stop your antidepressants without talking to your doctor. Stopping suddenly can be more dangerous than continuing. Sertraline (Zoloft) and citalopram (Celexa) are the most studied and considered safest during pregnancy. The risk of untreated depression-like poor nutrition, missed prenatal visits, or preterm birth-is often higher than the medication risk. Work with your provider to find the lowest effective dose.
Next Steps: What to Do Today
Don’t wait until you’re sick. Here’s what to do now:
- Check your medicine cabinet. Toss any expired or unnecessary OTC meds-especially multi-symptom cold pills.
- Write down every medication you take daily, including vitamins, supplements, and herbal products.
- Bring that list to your next prenatal visit. Ask: “Which of these are safe? Which should I stop?”
- Download the FDA’s “Medicines in Pregnancy” app. It’s free, updated regularly, and doesn’t require an account.
- Keep a small notebook. Note when you take a medication, why, and how you felt. It helps your provider spot patterns.
Pregnancy isn’t the time to wing it. But it’s also not the time to suffer in silence. With the right information, you can stay healthy-without putting your baby at risk.






Comments (13)
Peyton Feuer
4 Jan 2026
this is actually super helpful. i was about to grab some advil for my headache until i saw this. tylenol it is. also didn't know about the miralax thing, gonna stock up.
Angie Rehe
4 Jan 2026
ACOG guidelines are outdated. The MotherToBaby registry is a corporate front. They don't track long-term neurodevelopmental outcomes. You think acetaminophen is safe? Try asking the kids with ADHD born to moms who took it weekly. The FDA's own data shows a 30% increased risk of ASD with prenatal exposure. They just don't label it because lawsuits.
josh plum
6 Jan 2026
you people are terrifying. i took zyrtec for 8 months pregnant and my kid is 7 and aced the gifted test. but you wanna scare everyone with 'neurodevelopmental risks'? that's fearmongering. if you're that scared, stay off the internet and go meditate.
John Ross
7 Jan 2026
The pharmacokinetic profile of guaifenesin demonstrates negligible placental transfer due to its high molecular weight and low lipid solubility. This is corroborated by the 2023 ACOG Practice Bulletin No. 218. Avoid combination products containing phenylephrine - it's a potent alpha-1 agonist that induces uterine vasoconstriction. Stick to monotherapy.
Siobhan Goggin
8 Jan 2026
I wish more doctors would give out lists like this. I spent weeks Googling and crying because I didn't know if ginger tea was okay. This is the kind of clarity pregnant people need.
Ashley Viñas
10 Jan 2026
of course you're recommending unisom. because that's what big pharma wants you to take. did you know doxylamine is a derivative of diphenhydramine? it's an antihistamine that crosses the blood-brain barrier. they don't test on pregnant women because they know what happens. you're normalizing chemical sedation for morning sickness. shame.
Shanna Sung
12 Jan 2026
they're hiding the truth. acetaminophen is linked to autism. the FDA knows. the CDC knows. the pharmaceutical industry pays the researchers. i took it twice and my daughter has sensory issues. they won't tell you because they make billions. check the FDA's yellow card reports. they're not public but i got them from a whistleblower
Clint Moser
13 Jan 2026
i think the real danger is not the meds but the fact that you have to read 1000 words to figure out if tylenol is ok. why is this so complicated? why can't my ob just give me a card? i think the system is designed to make us feel stupid and scared. i just want to sleep.
Mandy Kowitz
14 Jan 2026
so basically if you're pregnant you can't take anything without a 12-page risk assessment? i'm just gonna drink bleach. it's natural and it'll solve my headache faster than any of this nonsense.
Michael Rudge
14 Jan 2026
i read this whole thing and i'm still not sure if i can take a single ibuprofen. i guess i'll just suffer like a medieval peasant. meanwhile my husband is taking nyquil like candy. patriarchy much?
mark etang
16 Jan 2026
Esteemed contributors, I commend the meticulous curation of evidence-based pharmacological data herein. The integration of ACOG, CDC, and MotherToBaby registries constitutes a paradigmatic advancement in maternal-fetal therapeutics. I urge all expectant individuals to retain this document in their prenatal binder, alongside the ultrasound photos and birth plan. Knowledge is the most potent prophylactic.
Justin Lowans
16 Jan 2026
this is the kind of resource i wish existed when i was pregnant. i took everything 'natural' because i thought it was safer - turned out i ate a bunch of chamomile tea that probably messed with my hormones. i'm so glad someone finally laid it out plain. no fluff, no fear, just facts. thank you.
Jason Stafford
16 Jan 2026
THEY'RE LYING. THEY ALWAYS LIE. I WORKED AT A PHARMACY. I SAW THE INTERNAL MEMOS. THE FDA KNEW ABOUT THE ASHES OF THE BABIES. THEY DON'T WANT YOU TO KNOW THAT ACETAMINOPHEN BREAKS DOWN INTO TOXIC METABOLITES THAT CROSS THE PLACENTA AND STICK TO THE FETAL BRAIN. THEY'RE SELLING POISON IN WHITE PILLS AND CALLING IT SAFE. I'VE BEEN SILENCED BEFORE. I WON'T BE SILENCED AGAIN.