CYP450 Enzyme Interactions: How Medications Compete for Metabolism

Imagine taking two pills at the same time - one for your blood pressure, another for your depression - and not realizing they’re fighting over the same enzyme in your liver. One wins. The other doesn’t get broken down. Suddenly, you’re flooded with too much of one drug. Or worse - neither works because they both got blocked. This isn’t science fiction. It’s happening right now in millions of people’s bodies every day. The reason? CYP450 enzymes.
What Are CYP450 Enzymes, Really?
CYP450 enzymes are a group of proteins in your liver and intestines that act like molecular scissors. Their job? Cut up drugs so your body can flush them out. About 90% of all prescription medications rely on these enzymes to be processed. That’s not a small number - it’s the backbone of how your body handles medicine.
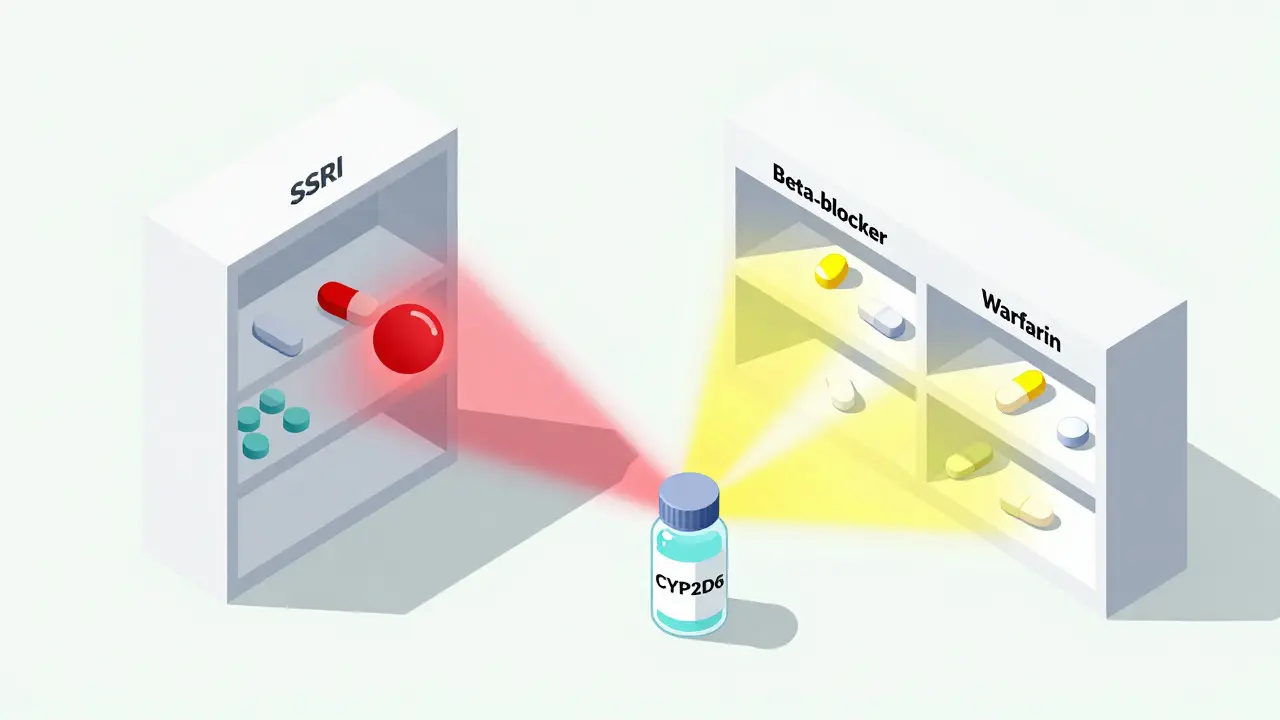
There are six main types that do most of the work: CYP3A4, CYP2D6, CYP2C9, CYP2C19, CYP1A2, and CYP2E1. Together, they handle nearly every drug you’ve ever taken. CYP3A4 alone is responsible for breaking down half of all medications - from statins to antibiotics to painkillers. CYP2D6 handles a quarter, including most antidepressants and beta-blockers. If you’re on any of these, you’re already in the mix.
These enzymes don’t work in a vacuum. They’re crowded. Imagine a single toll booth with 50 cars trying to get through at once. Some cars are faster. Some are bigger. Some block the lane on purpose. That’s what happens when two drugs compete for the same enzyme.
How Do Drugs Compete? Inhibition and Induction
There are two main ways one drug messes with another’s metabolism: inhibition and induction.
Inhibition is like cutting the brake lines on a rival car. One drug latches onto the enzyme and blocks others from using it. This can happen fast - sometimes within hours. For example, if you take clarithromycin (an antibiotic) with simvastatin (a cholesterol drug), the antibiotic clamps down on CYP3A4. Simvastatin can’t break down. It builds up. Levels can spike 10 times higher. That’s how a simple combo led to rhabdomyolysis - muscle breakdown so severe it damaged kidneys in a 72-year-old woman. It’s not rare. It’s predictable.
Some inhibitors are stronger than others. Ketoconazole? It’s a heavyweight. It can make a drug’s concentration jump 5 to 10 times. Grapefruit juice? Yes, really. It blocks CYP3A4 in the gut. One glass can reduce drug clearance by 30% to 80%. That’s why you see warnings on statin bottles: “Avoid grapefruit.”
Induction is the opposite. It’s like building a whole new toll booth. Rifampin, an antibiotic used for tuberculosis, tells your liver to make more CYP3A4 enzymes. Suddenly, your body becomes a drug-processing machine. If you’re on birth control, an antiviral, or even a blood thinner, the drug gets broken down too fast. It stops working. A patient on warfarin who starts rifampin might end up with a blood clot because the anticoagulant vanished from their system.
Induction takes time - days to weeks - and lasts even longer after you stop. That’s why interactions don’t always show up right away. You might feel fine for a week… then crash.
Genes Matter More Than You Think
Not everyone metabolizes drugs the same way. Your genes decide whether you’re a slow, normal, or super-fast processor.
For CYP2D6, about 5-10% of white people are poor metabolizers. That means their bodies barely touch certain drugs. Take codeine. It’s a prodrug - it needs CYP2D6 to turn into morphine. If you’re a poor metabolizer? You get no pain relief. If you’re an ultrarapid metabolizer? You turn codeine into morphine so fast it floods your system. That’s how a healthy teen died after a routine tonsillectomy - standard dose, genetic surprise.
Same goes for antidepressants. CYP2D6 poor metabolizers need 50% less of drugs like amitriptyline or paroxetine. Give them the normal dose? They get dizzy, nauseous, or worse. But if you don’t test for it? You’re guessing.
Genetic testing for CYP2D6, CYP2C19, and others is now available. Hospitals in the U.S. are starting to use it - especially for clopidogrel (a blood thinner). About 30% of Caucasians and 60% of Asians are poor metabolizers of this drug. If they get the standard dose? Their heart attack risk doesn’t drop. They need a different drug. Testing costs $250-$500. But compared to a heart attack? It’s cheap.

Real Cases, Real Consequences
It’s not theoretical. Nurses see this daily.
A 2023 survey of 1,200 nurses found that 15-20% of patients on SSRIs like fluoxetine or paroxetine - which block CYP2D6 - and beta-blockers like metoprolol developed dangerously slow heart rates. The SSRI blocked the metabolism of metoprolol. The drug piled up. The heart slowed. Some patients needed hospitalization.
Another case: a man on theophylline (for asthma) started fluvoxamine (an antidepressant). Fluvoxamine is a strong CYP1A2 inhibitor. Within 48 hours, theophylline levels jumped from 10 to 25 mcg/mL. Normal range is 10-20. He had a seizure. He survived. But only because someone caught it.
And then there’s St. John’s wort. People think it’s “natural,” so it’s safe. It’s not. It’s a powerful CYP3A4 inducer. It can slash levels of cyclosporine, birth control, and even HIV meds by half. One woman got pregnant because her birth control stopped working after taking the supplement for “mild depression.”
What Can You Do?
You don’t need to be a pharmacist to avoid these traps. Here’s what actually works:
- Know your meds. If you’re on five or more drugs, you’re at high risk. The average Medicare patient takes 5.4 medications - that’s over 10 potential CYP450 clashes.
- Ask your pharmacist. Pharmacists check for these interactions daily. They use tools like Lexicomp, which catches 95% of major ones. Don’t assume your doctor knows every interaction. Most don’t.
- Check for red flags. Is a new drug labeled “avoid with grapefruit”? “May increase levels of other drugs”? “Use with caution”? That’s your cue to dig deeper.
- Don’t skip the supplement check. Herbs, vitamins, even green tea can interfere. St. John’s wort, goldenseal, and curcumin all mess with CYP enzymes.
- Consider testing. If you’ve had unexplained side effects, or if a drug never worked for you - even at normal doses - ask about pharmacogenomic testing. It’s not sci-fi. It’s becoming standard.
The Bigger Picture
CYP450 interactions cause about 30% of all adverse drug events. That’s 1 in 3 bad reactions from meds. And they’re preventable. The FDA now requires drug labels to list CYP450 interactions. Over 90% of new drugs approved in 2022 included these warnings.
Hospitals are catching up. 65% of U.S. hospitals now have some kind of CYP450 safety protocol. EHR systems like Epic and Cerner now pop up alerts when a dangerous combo is prescribed. But only 28% of primary care doctors check for these regularly. That’s a gap.
The future? AI. IBM Watson’s drug interaction tool is already in beta, predicting CYP450 clashes with 89% accuracy. The NIH is standardizing gene names so labs worldwide speak the same language. By 2025, we’ll have clearer rules for genetic testing.
But right now? The system still relies on you - the patient - to speak up. To ask questions. To say, “I’m taking this - is it safe with that?”
Because when two drugs fight over one enzyme, someone always loses. It doesn’t have to be you.
What are the most common CYP450 enzyme interactions?
The most frequent and dangerous interactions involve CYP3A4 and CYP2D6. CYP3A4 is involved with statins (like simvastatin), calcium channel blockers, and many opioids - and it’s easily blocked by antibiotics like clarithromycin or grapefruit juice. CYP2D6 handles many antidepressants and beta-blockers; SSRIs like fluoxetine or paroxetine can inhibit it, causing dangerous buildup of metoprolol or propranolol. Another major one is CYP2C9 and warfarin, where drugs like amiodarone or fluconazole can spike bleeding risk.
Can over-the-counter drugs cause CYP450 interactions?
Absolutely. Common OTCs like ibuprofen (CYP2C9 inhibitor), diphenhydramine (CYP2D6 inhibitor), and even some antifungal creams (like clotrimazole) can interfere. St. John’s wort - often sold as a natural mood booster - is one of the most dangerous, as it strongly induces CYP3A4 and can make birth control, immunosuppressants, and HIV drugs fail. Even large doses of vitamin C or green tea extract can affect CYP1A2.
How long do CYP450 interactions last?
It depends. Reversible inhibition (like grapefruit juice or fluoxetine) lasts as long as the inhibitor is in your system - usually a few days. Irreversible inhibition (like clarithromycin) takes 3-7 days for your liver to make new enzymes. Induction (like rifampin or St. John’s wort) takes 3-14 days to kick in and can last 1-3 weeks after stopping. That’s why timing matters - you can’t just skip a dose and assume safety.
Is pharmacogenomic testing worth it?
If you’ve had bad reactions to multiple drugs, or if standard doses don’t work for you, yes. Testing for CYP2D6, CYP2C19, and CYP2C9 can explain why a drug failed or caused side effects. It’s especially valuable for antidepressants, blood thinners, and pain meds. Costs are $250-$500, and results take 3-7 days. Many insurers cover it if you’re on multiple high-risk meds. It’s not a magic bullet - but it removes guesswork.
Can CYP450 interactions be avoided entirely?
You can’t avoid them completely - because your body needs to process drugs. But you can avoid the dangerous ones. Always tell your doctor and pharmacist about every pill, patch, herb, and supplement. Use interaction checkers like Lexicomp or Micromedex. Ask: “Is this safe with my other meds?” Don’t assume it’s fine because it’s “natural” or “over-the-counter.” Most serious interactions come from things people think are harmless.
Next Steps: What to Do Today
If you’re on three or more medications, take five minutes right now:
- Write down every drug and supplement you take - including vitamins and herbal teas.
- Check each one against a trusted interaction tool (like Medscape’s Drug Interaction Checker or the FDA’s database).
- Call your pharmacist and ask: “Are any of these competing for the same enzyme?”
- If you’ve had unexplained side effects or drug failures, ask your doctor about CYP450 genetic testing.
Medications aren’t just chemicals. They’re signals in a crowded system. And if you don’t know how they’re being processed - you’re flying blind.






Comments (11)
Louis Paré
30 Dec 2025
So let me get this straight - we’re giving people cocktails of drugs that fight like alley cats over a single enzyme, then acting shocked when someone ends up in the ER? This isn’t medicine. It’s Russian roulette with a prescription pad. And don’t even get me started on how pharmacists are the only ones paying attention while doctors scroll through TikTok between visits.
Marie-Pierre Gonzalez
30 Dec 2025
Thank you for this incredibly important post 🙏 I’ve seen so many patients suffer from these hidden interactions - especially the elderly on 7+ meds. I’ll be sharing this with my entire care team. Please keep writing like this - it saves lives. 💙
Janette Martens
30 Dec 2025
Why do we even allow these drugs to be sold if they’re this dangerous? In Canada we don’t let junk food be marketed to kids - why the hell are we letting pharma poison people with combos that are known to kill? Someone’s gotta get sued for this.
Manan Pandya
1 Jan 2026
This is one of the clearest explanations of CYP450 interactions I’ve ever read. The toll booth analogy alone is worth a thousand textbooks. I work in a rural clinic in India where patients often combine Ayurvedic herbs with Western meds - and no one checks for interactions. This needs to be translated and distributed widely.
Aliza Efraimov
2 Jan 2026
OH MY GOD. I was on fluoxetine and metoprolol for YEARS and never knew why I was so dizzy all the time. I thought it was just aging. I almost died. I just called my pharmacist and they pulled the interaction right away. This post literally saved me. I’m crying. Thank you.
Paige Shipe
2 Jan 2026
Interesting. But let’s be honest - most people don’t even know what a CYP enzyme is. This is like teaching quantum physics to toddlers. The system is broken, and no amount of awareness will fix it when profit drives prescribing. You think a CEO cares if grandma gets rhabdomyolysis? Nope.
Tamar Dunlop
3 Jan 2026
As a nurse practitioner in Toronto, I can confirm: the most dangerous interactions are not the flashy ones - they’re the quiet ones. The patient taking St. John’s Wort for ‘mild anxiety’ while on warfarin. The grandmother popping turmeric capsules because ‘it’s anti-inflammatory’ - unaware it’s inhibiting CYP2C9. These are the silent killers. Education must begin at the pharmacy counter - not the ER.
Emma Duquemin
4 Jan 2026
Imagine if your car had 10 different fuel systems, all jostling for the same gas line - and the manual said ‘use whatever you want.’ That’s our body. And we’re all just winging it. I just Googled my meds and found out my morning coffee is slowing down my antidepressant. I’m switching to tea. And yes, I’m telling my doctor. This isn’t just science - it’s survival.
Kevin Lopez
5 Jan 2026
CYP3A4 substrate + inhibitor = elevated AUC. CYP2D6 PM = poor efficacy. Induction = reduced Cmax. These are not mysteries. They’re pharmacokinetic 101. If you’re prescribing without checking Lexicomp, you’re negligent. Period.
Samar Khan
6 Jan 2026
So… if I take CBD oil with my blood pressure med… am I basically playing Russian roulette? 🤡 I just got my first prescription last week and now I’m scared to take anything. Why is no one talking about this??
Russell Thomas
7 Jan 2026
Wow. So the real problem isn’t the drugs - it’s the people who think ‘natural’ means ‘safe.’ St. John’s Wort? More like St. John’s Death Wish. And don’t get me started on people who take melatonin with antidepressants and wonder why they’re hallucinating. Wake up. Your supplement aisle is a minefield.