Polypharmacy Risk Checklist: Spot Dangerous Drug Combos Before It’s Too Late

Taking five or more medications every day isn’t just common-it’s becoming the norm for older adults. In the U.S., over a third of people in their 60s and 70s are on five or more prescriptions. And while some of these drugs save lives, others are quietly setting the stage for falls, confusion, hospital visits, or worse. The problem isn’t always the drugs themselves. It’s what happens when they’re mixed together.
Why Polypharmacy Isn’t Just About Quantity
Polypharmacy means more than just having a lot of pills. It’s about the hidden risks when those pills interact. A single medication might be fine on its own. But add a second, then a third, and suddenly your body’s chemistry gets thrown off. The CDC says nearly 1.3 million emergency room visits each year are caused by bad drug reactions-and most of them happen in people over 65. And it’s not just prescriptions. Over-the-counter painkillers, sleep aids, herbal supplements, even grapefruit juice can turn a safe regimen into a dangerous one.One man in Sheffield, 72, started taking a daily blood pressure pill, then added a common OTC cold remedy for a cough. Within days, he was dizzy, nearly fell down the stairs, and ended up in A&E. His doctor later found the combo raised his blood pressure instead of lowering it. That’s not rare. It’s predictable.
The Top 5 High-Risk Combinations You Need to Know
Some drug pairs are so risky they’re flagged in clinical guidelines. Here are the ones that cause the most harm:- Warfarin + cranberry juice: Warfarin thins your blood. Cranberry juice makes it thinner-way too thin. This combo can lead to internal bleeding, even from a minor bump.
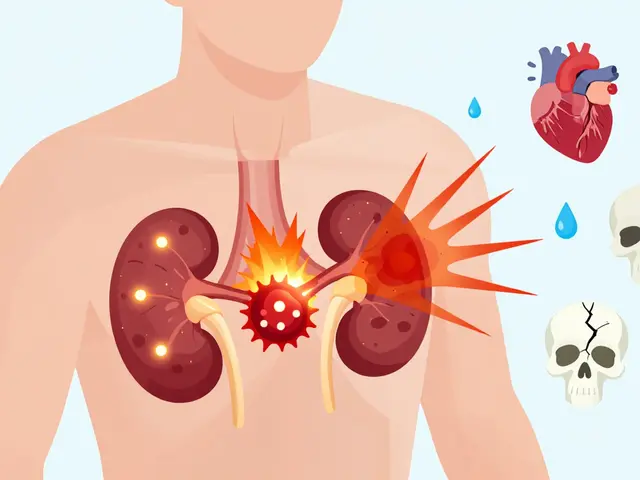
- Statins + grapefruit juice: Statins like atorvastatin help lower cholesterol. Grapefruit blocks the enzyme that breaks them down. That means too much drug builds up in your system, risking muscle damage (rhabdomyolysis), which can wreck your kidneys.
- Blood pressure meds + decongestants (like pseudoephedrine): Decongestants are in most cold and allergy meds. They tighten blood vessels-which is the opposite of what your blood pressure pill is trying to do. Result? Sudden spikes in pressure, stroke risk.
- Acetaminophen + oxycodone + prochlorperazine: This trio is common after surgery or chronic pain. But together, they cause extreme drowsiness, confusion, and breathing trouble. Studies show this combo shows up in ER visits far more than chance would explain.
- Benzodiazepines (like diazepam) + opioids (like oxycodone): Both depress the central nervous system. Together, they slow breathing to dangerous levels. The CDC lists this as one of the deadliest combinations in older adults.
And don’t forget calcium supplements. They’re often taken with blood pressure meds like lisinopril or diuretics like furosemide. In large doses, calcium can interfere with how these drugs work-or cause kidney stones.
The Beers Criteria: Your Secret Weapon Against Bad Prescriptions
Doctors don’t always know which drugs are risky for older patients. That’s where the Beers Criteria comes in. Updated in 2019, it’s a trusted list of medications that should be avoided-or used with extreme caution-in people over 65. It’s not about banning drugs. It’s about recognizing when the risks outweigh the benefits.Here’s what the Beers Criteria flags as especially dangerous:
- Anticholinergic drugs (like diphenhydramine/Benadryl, oxybutynin): These cause confusion, memory loss, dry mouth, constipation. They’re in many sleep aids, allergy pills, and bladder meds.
- Benzodiazepines (like lorazepam, alprazolam): Even short-term use increases fall risk by 50%.
- Alpha-blockers (like doxazosin): Used for prostate issues, but they drop blood pressure too much when standing up-leading to fainting.
- NSAIDs (like ibuprofen, naproxen): Can cause kidney failure or stomach bleeding, especially when taken with blood thinners or diuretics.
Ask your doctor: "Is this drug on the Beers list? Is there a safer alternative?" If they don’t know, it’s time to find a provider who does.

Prescribing Cascades: The Hidden Trap
One of the sneakiest dangers isn’t the drugs themselves-it’s how they’re added. A prescribing cascade happens when a side effect from one drug is treated with another drug, which causes another side effect, and so on.Example: You take an opioid for pain → it causes constipation → your doctor prescribes a laxative → the laxative causes electrolyte imbalance → now you need potassium supplements → and so on. Suddenly, you’re on 12 pills instead of 3.
A 2023 study at the University of Rochester found that nearly 40% of older patients on multiple meds were caught in this cycle. And no one noticed-because each new drug was "fixing" a problem created by the last one.
Break the cycle by asking: "What was this drug originally prescribed for? Is it still needed?" If the answer is vague or "just in case," it’s time to reconsider.
Your Polypharmacy Risk Checklist: Do This Now
You don’t need a PhD to protect yourself. Use this simple checklist every time you see a doctor or pharmacist:- Make a full list-include every prescription, OTC medicine, vitamin, herb, and supplement. Don’t forget patches, eye drops, or inhalers.
- Bring it to every appointment. Don’t rely on memory. Write it down. Use a free app like Medisafe or MyTherapy if it helps.
- Ask: "Is this still necessary?" For each drug, ask your doctor: "Why am I taking this? What happens if I stop?"
- Check for Beers Criteria drugs. If you’re on any listed above, ask for alternatives.
- Ask about food interactions. Grapefruit? Cranberry? Alcohol? Dairy? These aren’t just warnings-they’re red flags.
- Request a pharmacist review. Pharmacists are trained to spot interactions. Ask for a free medication review at your local pharmacy.
- Track side effects. Write down dizziness, confusion, fatigue, or falls. Bring this list to your next visit.
Some people think deprescribing means giving up treatment. It doesn’t. It means removing what’s unnecessary. One cancer patient on the CancerCare forum reduced his meds from 12 to 7 using the ARMOR method-Assess, Review, Minimize, Optimize, Reassess. He felt clearer, slept better, and had fewer falls.
Who Should Be on This Checklist?
This isn’t just for the elderly. Anyone taking five or more medications should use it. That includes people with:- Heart disease, diabetes, or kidney disease
- Chronic pain or mental health conditions
- Cancer or autoimmune disorders
- Multiple specialists (cardiologist, neurologist, rheumatologist, etc.)
The more doctors you see, the higher the risk. One doctor doesn’t know what another prescribed. That’s why you need to be the quarterback of your own care.

What’s Changing in 2026?
Health systems are starting to catch up. The WHO’s Medication Without Harm initiative aims to cut severe drug harm by 50% by 2027. Some hospitals now use AI tools to flag risky combinations in real time. Smart pill bottles track if you’re taking meds correctly. Genetic tests can show if you metabolize drugs slowly-making you more vulnerable to side effects.But tech won’t fix this alone. The real solution is you-asking questions, keeping lists, and refusing to accept "it’s just part of getting older." You have the right to be safe.
When to Call for Help
If you or a loved one has experienced:- Falling more than once in 6 months
- Confusion or memory lapses that started after a new medication
- Unexplained fatigue or nausea
- Emergency room visits linked to medication use
Don’t wait. Schedule a medication review. Talk to a pharmacist. Ask for help. You don’t have to manage this alone.
What is polypharmacy, and why is it dangerous?
Polypharmacy means taking five or more medications regularly. It’s dangerous because each additional drug increases the chance of harmful interactions-like dizziness, falls, kidney damage, or internal bleeding. Older adults are especially at risk because their bodies process drugs differently.
Can over-the-counter drugs cause dangerous interactions?
Yes. Common OTC meds like Benadryl, ibuprofen, and cold remedies can interact badly with prescriptions. For example, taking pseudoephedrine (in decongestants) with blood pressure meds can spike your blood pressure. Even herbal supplements like St. John’s Wort can make antidepressants or blood thinners less effective-or more toxic.
What is the Beers Criteria, and should I check my meds against it?
The Beers Criteria is a list of medications that are risky for older adults, updated every few years by experts. It flags drugs like benzodiazepines, anticholinergics, and NSAIDs that can cause confusion, falls, or organ damage. If you’re over 65 and on multiple meds, you should review your list against it. Ask your doctor or pharmacist to do it with you.
How can I tell if a drug is causing side effects?
Watch for new symptoms that started after adding a drug: dizziness, confusion, fatigue, constipation, nausea, or falls. Keep a simple journal: write down what you took, when, and how you felt. Bring it to your next appointment. Many side effects are mistaken for aging-but they’re often drug-related.
Can I stop taking some of my meds on my own?
Never stop a prescription without talking to your doctor. Some drugs need to be tapered slowly to avoid withdrawal or rebound effects. But you can-and should-ask if any meds are still necessary. Many are taken "just in case" or out of habit. A pharmacist can help you identify which ones might be safe to reduce or stop.
Do pharmacists really help with medication reviews?
Yes. Pharmacists are trained to spot drug interactions, food conflicts, and duplicate therapies. In the UK, many pharmacies offer free medication reviews-no appointment needed. Bring your full list, including supplements. They’ll tell you what’s risky and what can be simplified. It’s one of the most underused safety tools available.
Next Steps: Start Today
Grab a pen. Write down every pill, patch, drop, and supplement you take. Don’t skip the vitamins or herbal teas. Then, call your pharmacy or GP and ask for a medication review. Say: "I’m on several drugs. I want to make sure they’re still safe together." You don’t need to be sick to do this. You just need to be smart.Medications are powerful. Used right, they heal. Used wrong, they hurt. You’re not just a patient-you’re the one who holds the list. Keep it updated. Ask the hard questions. And don’t let anyone tell you that taking a lot of pills is just part of getting older. It’s not. It’s a risk-and one you can control.





Comments (9)
sagar sanadi
19 Jan 2026
lol so now we're scared of pills? next they'll say water is dangerous when mixed with salt. i've been taking 12 meds since 2015 and i still beat my grandpa at chess. he died at 92 with 17 prescriptions and a cat named billy. who's the real victim here? the system? or the people who actually live?
kumar kc
21 Jan 2026
People die because they don't ask questions. This isn't fearmongering-it's basic responsibility.
clifford hoang
22 Jan 2026
They don't tell you this but the FDA and Big Pharma fund these 'Beers Criteria' studies... 🤫 the real goal? get you off cheap meds so you buy their new $800/month 'solution'. also... grapefruit juice is a natural blood thinner. it's not the juice-it's the lab-made drugs that can't handle nature. 🍊💉 #pharmacracy
Jacob Cathro
22 Jan 2026
ok but like... why are we even talking about this? like i get it, drugs are scary. but my aunt took 14 pills and still went skydiving at 78. also... who wrote this? a pharmacist who hates fun? 🤡 i just want to nap without getting a lecture about rhabdomyolysis
Paul Barnes
24 Jan 2026
The article is well-researched and accurately reflects clinical guidelines. The Beers Criteria are evidence-based, and prescribing cascades are a documented phenomenon in geriatric pharmacology. Ignoring these risks is not autonomy-it's negligence.
pragya mishra
25 Jan 2026
I called my mom's doctor last week and told him he's killing her with all these pills. He said 'she's 81, what do you expect?' I said 'expect her to walk without falling!' He shut up. You need to be loud. They don't listen unless you scream.
Manoj Kumar Billigunta
25 Jan 2026
This is exactly why I started helping my neighbors with their med lists. No judgment. No drama. Just: 'Let's sit down, look at everything, and see what we can safely let go.' One guy cut his meds from 11 to 6. He said he finally remembered his wife's birthday. That’s the win. You don’t need to be a doctor to help someone live better.
Andy Thompson
26 Jan 2026
they want you scared so you take more pills. why do you think they push 'medication reviews'? it's a trap. they want you to feel guilty so you agree to MORE tests, MORE drugs, MORE $$$ for the system. america runs on pills. and you're just the ATM. 🇺🇸💊 #stopthefeed
Thomas Varner
27 Jan 2026
I’ve been on six meds for ten years… and honestly? I stopped checking. I just take them. I don’t even know why anymore. I mean… I guess they’re supposed to keep me alive? But I don’t feel alive… I just feel… like a pharmacy. 🤔 I’m not even mad. Just… tired.