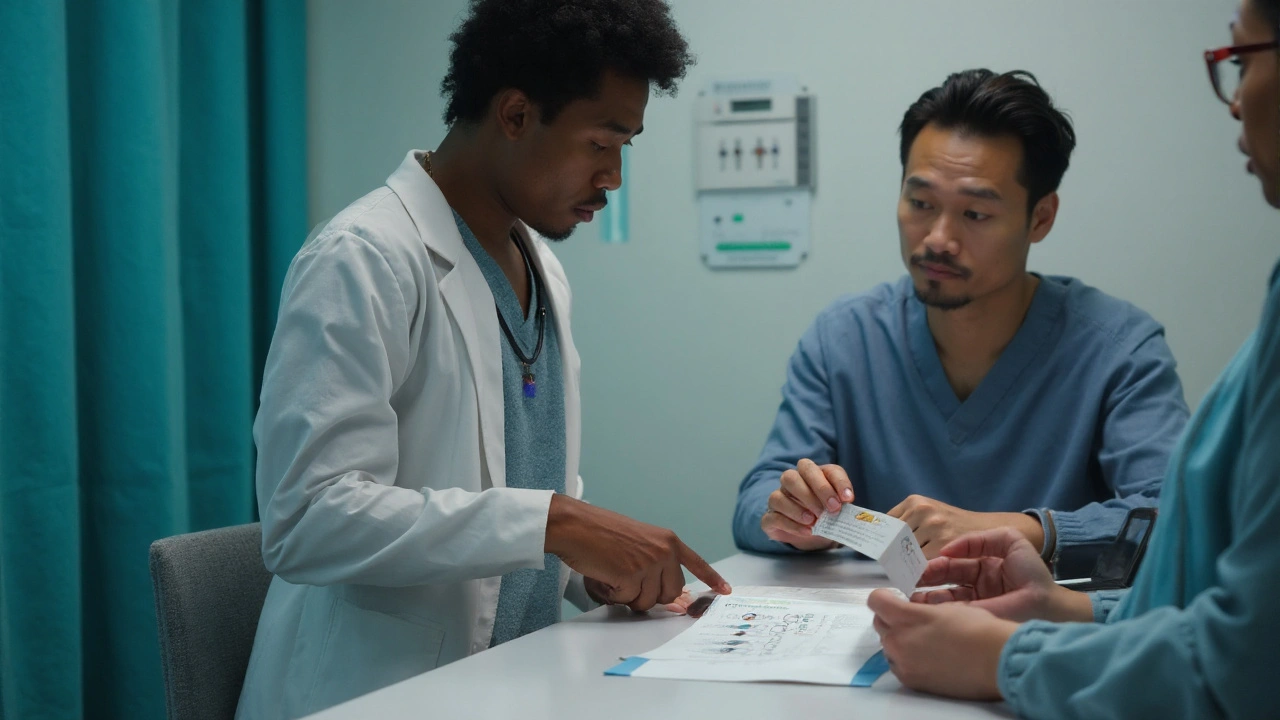
Apixaban and Heart Failure: Risks, Benefits, Dosing, and Safety Tips

Heart failure raises your risk of blood clots and stroke, but not everyone with heart failure needs a blood thinner. If your doctor mentioned apixaban, you probably want one thing: clarity. Who actually needs it? Is it safer than warfarin? How do you take it right-without turning everyday life into a bleeding-risk minefield? Here’s a plain‑English guide that answers those exact questions and helps you make smart, safe choices with your care team.
- TL;DR: In heart failure, apixaban is most often used when you also have atrial fibrillation (AF) or a blood clot (like DVT/PE). It lowers stroke risk versus no anticoagulant and has less brain bleeding than warfarin in trials.
- It is not used just because you have heart failure. No AF and no clot? You usually don’t need a blood thinner.
- Typical AF dose is 5 mg twice daily; it’s reduced to 2.5 mg twice daily if you meet 2 of these: age ≥80, weight ≤60 kg, serum creatinine ≥1.5 mg/dL.
- Watch for bleeding (black stools, vomiting blood, new severe headache). Avoid mixing with NSAIDs and certain antibiotics/antifungals without clearance.
- Before procedures, you’ll likely pause it for 1-3 days depending on bleeding risk and your kidneys. Ask your team for a written plan.
When apixaban makes sense in heart failure
Apixaban is an oral anticoagulant (a “blood thinner”). It blocks Factor Xa to reduce clot formation. In heart failure, the key is matching the medicine to the right problem. That means knowing when it helps, and when it doesn’t.
apixaban is usually prescribed in heart failure for three situations:
- Atrial fibrillation (AF): AF plus heart failure multiplies stroke risk. The 2023 ACC/AHA guidelines prefer direct oral anticoagulants (DOACs) like apixaban over warfarin for most people with nonvalvular AF, except if you have a mechanical heart valve or moderate-to-severe rheumatic mitral stenosis.
- Deep vein thrombosis (DVT) or pulmonary embolism (PE): It treats the clot now and prevents another one later. This is common after hospitalization, immobility, or active cancer.
- Left ventricular (LV) thrombus or other special clots: After a big heart attack or with very weak heart pumping, a clot can form inside the heart. Warfarin has been the traditional choice, but real-world data are growing for DOACs; decisions here are individualized.
When does apixaban not help in heart failure?
- Heart failure without AF or a clot: Large trials of anticoagulation in heart failure patients who are in normal rhythm didn’t show a net benefit (e.g., WARCEF for warfarin vs aspirin; COMMANDER-HF with rivaroxaban). So if you have heart failure but no AF and no clot, you usually don’t need a blood thinner.
- Mechanical heart valves or rheumatic mitral stenosis: Use warfarin, not a DOAC.
Why apixaban over warfarin in AF? In the ARISTOTLE trial, apixaban cut stroke/systemic embolism versus warfarin and lowered major bleeding and death. This held true in the heart failure subgroup. Multiple meta-analyses since then show DOACs generally reduce intracranial hemorrhage compared with warfarin. That safety edge matters in a population where falls, frailty, and kidney swings are common.
How do you know if you need it with AF? Clinicians use the CHA₂DS₂-VASc score to estimate stroke risk. Heart failure or low ejection fraction adds 1 point. As a rule of thumb in 2025:
- Men: anticoagulate at score ≥2; consider at 1 (discuss nuances like bleeding risk).
- Women: anticoagulate at score ≥3; consider at 2.
Put simply: If you have heart failure and AF, you’re usually in the anticoagulation zone unless there’s a strong reason not to be.
Quick decision guide (talk this through with your cardiologist):
- HF + AF + CHA₂DS₂-VASc in treatment range → apixaban preferred over warfarin (unless mechanical valve/rheumatic MS).
- HF + recent DVT/PE → apixaban is a guideline-recommended option.
- HF + LV thrombus → shared decision; warfarin is classic, DOACs increasingly used off‑label.
- HF but no AF and no clot → skip anticoagulation; focus on heart failure therapy that saves lives (beta‑blocker, ACEi/ARB/ARNI, MRA, SGLT2 inhibitors, etc.).
Evidence snapshot (no links, just names you can look up): ARISTOTLE (apixaban vs warfarin in AF); AUGUSTUS (apixaban in AF with ACS/PCI, less bleeding without aspirin); AMPLIFY (apixaban for DVT/PE); ANNEXA‑4 (andexanet alfa reversal); 2023 ACC/AHA/HRS AF Guideline; 2022 AHA/ACC/HFSA Heart Failure Guideline; 2021 ISTH guidance on DOACs in obesity.

How to take it safely: dosing, interactions, labs, and procedures
Standard AF dosing: 5 mg by mouth twice daily.
Use 2.5 mg twice daily if you meet at least two of these: age ≥80 years, body weight ≤60 kg, or serum creatinine ≥1.5 mg/dL. Your team may also reduce the dose in advanced kidney disease or if you’re on strong drug interactions.
VTE dosing (typical):
- Treatment phase: 10 mg twice daily for 7 days, then 5 mg twice daily.
- Extended prevention after at least 6 months: 2.5 mg twice daily is common.
Kidneys, liver, and your heart failure:
- Heart failure can swing kidney numbers with diuretic changes or illness. That can change your bleeding risk. Get periodic labs and call if you notice swelling or dehydration.
- Moderate-to-severe liver disease can raise apixaban levels; dosing or drug choice may change.
Danger signs of bleeding-call now or go to urgent care/ER:
- Black or tarry stools; bright red blood per rectum
- Vomiting blood or coffee-ground material
- Coughing up blood; pink frothy sputum with bleeding signs
- New, severe, or “worst-ever” headache; vision changes; one-sided weakness
- Fainting or persistent dizziness; unusual, large bruises
Common side effects include easy bruising, nosebleeds, gum bleeding. If they’re frequent or heavy, tell your team-there are ways to tune the plan.
Missed dose rule (twice‑daily regimen): Take it as soon as you remember the same day, then take the next dose at the usual time. Don’t double up.
Interactions to keep on your radar (apixaban is affected by P‑gp/CYP3A4):
- Strong inhibitors (raise levels, increase bleeding): ketoconazole, itraconazole, posaconazole, voriconazole; ritonavir-boosted antivirals (e.g., nirmatrelvir/ritonavir for COVID); clarithromycin. Your team may reduce dose or choose a different plan.
- Strong inducers (lower levels, risk of clots): rifampin; carbamazepine; phenytoin; phenobarbital; St. John’s wort. Usually avoid together.
- Other blood thinners: aspirin, clopidogrel, ticagrelor, prasugrel raise bleeding risk. In AF plus recent stent, most patients use apixaban + a single antiplatelet (often clopidogrel) and drop aspirin early-this is backed by AUGUSTUS.
- NSAIDs: ibuprofen, naproxen, diclofenac increase bleeding; use acetaminophen for pain unless told otherwise.
- Herbals/supplements: fish oil and ginkgo can add bleeding risk; discuss any supplement you take. Avoid high‑dose turmeric/curcumin without approval.
- Grapefruit juice: can raise levels; regular heavy intake isn’t a great idea here.
- Alcohol: keep it light; binge drinking plus a blood thinner is a bad combo for falls and bleeds.
Procedures and surgeries (including dental work):
- Low bleeding risk (simple skin surgery, many dental procedures): often stop 24 hours before.
- Higher bleeding risk (major surgery, high‑risk endoscopy): often stop 48-72 hours before; longer if kidney function is poor.
- Bridging with heparin is usually not needed for DOACs.
- Restart timing depends on bleeding risk and wound healing, often 24-72 hours after.
Ask for a written peri‑procedure plan. It should list the last dose timing, when you restart, and who to call if there’s bleeding.
Reversal in emergencies: Hospitals may use andexanet alfa (specific reversal) or four‑factor prothrombin complex concentrate if you have life‑threatening bleeding. That’s why carrying a medication card or using a phone medical ID is smart.
Monitoring: No routine INR checks like warfarin. Still, get labs at least yearly (often every 3-6 months in heart failure): CBC (hemoglobin/platelets), BMP (kidneys), and sometimes liver panel. Bring your medication list to every visit.
Adherence tips that actually work:
- Use a morning/evening pillbox and anchor doses to habits (teeth brushing, breakfast).
- Set smartphone alarms. Travel? Set one in the destination time zone before you go.
- Refill with a 7-10 day cushion; mail order helps if transportation is hard.
- Tell one trusted person you’re on a blood thinner; they can help in a pinch.
Special populations, quick notes:
- Recent stent or heart attack with AF: Apixaban + clopidogrel and stop aspirin early reduces bleeding vs triple therapy (AUGUSTUS). Duration of any aspirin is short and personalized.
- Obesity: Standard dosing is generally fine even at high weights per ISTH guidance; some centers check drug levels in extreme cases.
- Pregnancy/breastfeeding: DOACs aren’t first‑line. If you’re planning pregnancy or become pregnant, call your team promptly-switching to heparin may be needed.
- Cancer: Apixaban is often used for cancer‑related VTE, but drug interactions and bleeding risks differ-oncology and cardiology should coordinate.
Day‑to‑day questions: checklists, scenarios, and a mini‑FAQ
Real life is where the details matter. Use these quick guides to avoid common pitfalls.
Starting apixaban with heart failure-5‑minute checklist
- Confirm why you’re on it (AF? DVT/PE? LV thrombus?).
- Know your dose and the reason if it’s reduced.
- List every medication and supplement you take; ask about risky combos.
- Ask about your lab schedule and who calls if results change dosing.
- Get a procedure plan in writing if anything is planned in the next 3 months.
- Set up reminders and a pillbox before the first dose.
“Sick day” rules (HF + apixaban)
- Vomiting/diarrhea for more than a day? You may miss doses and get dehydrated. Call for advice-don’t just stop on your own.
- New antibiotics or antivirals (like ritonavir‑boosted COVID treatments)? Check for interactions before the first dose.
- Sudden kidney change (less urine, big weight gain, very low blood pressure)? Let your team know; bleeding risk can shift.
If you fall or hit your head
- If you lose consciousness, have a severe headache, or any stroke sign (face droop, arm weakness, speech trouble), call emergency services.
- Even if you feel okay, head injuries on a blood thinner can bleed internally-seek medical evaluation.
Traveling with apixaban
- Carry it in your hand luggage with the original label and one spare dose pack.
- Use alarms in destination time. Twice‑daily dosing? Aim for 12 hours apart, but a 1-2 hour shift is usually fine.
- Long flights? Walk every 1-2 hours, stay hydrated. Your clot risk is already covered by the anticoagulant, but movement helps swelling and comfort.
Dental and minor procedures
- Most cleanings and simple fillings proceed without stopping. For extractions or implants, your dentist and cardiologist should coordinate.
- If told to hold a dose, ask exactly when to stop and when to restart-write it down.
Pain and fever
- Use acetaminophen first line. Avoid ibuprofen, naproxen, and high‑dose aspirin unless your prescriber says it’s necessary.
- If pain needs more than a day or two of meds, call for a safer plan.
Heart failure meds that pair well
- Guideline‑directed meds (ARNI/ACEi/ARB, beta‑blocker, MRA, SGLT2 inhibitor) reduce hospitalizations and death. They don’t clash with apixaban, but watch kidney function and potassium as usual.
- Diuretics (like furosemide) don’t interact directly, but dehydration ups bleeding risk. Aim for steady weights, steady labs.
Pitfalls to avoid
- Doubling doses after a miss-wrong for twice‑daily apixaban.
- Starting a new antibiotic or antifungal without checking interactions.
- Adding daily NSAIDs for joint pain-bleeding risk jumps.
- Stopping on your own before a procedure-timing matters and so does clot risk.
- Skipping lab checks for a year in a patient with changing kidney function-too risky.
Mini‑FAQ
- Is apixaban safer than warfarin? In AF, it caused fewer intracranial hemorrhages and less major bleeding in ARISTOTLE. It also didn’t require INR checks and had fewer food interactions.
- Do I need to avoid leafy greens? No vitamin K restrictions with apixaban. Eat your vegetables.
- Can I take it once daily? No. It’s designed for twice‑daily dosing to keep levels steady.
- What if my ejection fraction improves? If AF is still present and your stroke risk score is high, you usually stay on it. Re‑assess yearly with your cardiologist.
- Can I crush it? Yes, apixaban can be crushed and given in certain vehicles; confirm details with your pharmacist.
- Will it interact with my SGLT2 inhibitor? No direct interaction, but dehydration from SGLT2s can accentuate bleeding risk-stay hydrated and monitor.
- Does it thin my blood too much for vaccines? No. Use a small‑gauge needle and firm pressure after the shot.
Talking points for your next visit
- “What’s my exact reason for apixaban and my target duration?”
- “Does my kidney function or age suggest the reduced dose?”
- “If I need a dental extraction next month, what’s the hold/restart plan?”
- “Given my stent, how long will I stay on clopidogrel with apixaban?”
- “Which antibiotics or antifungals should I avoid?”
Bottom line for patients with heart failure: You don’t take apixaban just because of heart failure. You take it because you have AF or a clot risk that makes the benefits outweigh the bleeding risk. When that’s the case, it’s a strong, evidence‑backed choice-especially versus warfarin-so long as you respect the basics: the right dose, watchful eyes on interactions, and a clear plan for procedures and emergencies.
Credible sources behind this guide (for your own reading list): 2023 ACC/AHA/HRS Guideline for the Management of AF; 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure; ARISTOTLE (apixaban vs warfarin in AF); AUGUSTUS (AF with ACS/PCI); AMPLIFY (VTE); ANNEXA‑4 (andexanet reversal); ISTH guidance on DOACs in obesity; observational analyses of DOACs in LV thrombus. Your cardiologist or pharmacist can pull the exact reports if you want the details.



Comments (19)
Debra Cine
29 Aug 2025
Hey folks, just a quick heads‑up: if you’re on the reduced 2.5 mg dose, double‑check that you actually meet two of the criteria (age ≥ 80, weight ≤ 60 kg, creatinine ≥ 1.5 mg/dL). It’s easy to miss one and stay on the higher dose 💊. Also, keep a pillbox by your bedside so you don’t forget the evening dose. And yes, you can still have a slice of pizza 🍕 – just stay hydrated!
Rajinder Singh
3 Sep 2025
The recent ARISTOTLE trial data unequivocally demonstrate apixaban’s superiority over warfarin in reducing intracranial hemorrhage. When managing a heart‑failure patient with atrial fibrillation, the choice is clear: prefer the direct oral anticoagulant unless a mechanical valve is present. Ensure renal function is assessed at least biannually, as creatinine clearance directly influences dosing. In my practice, I also avoid concomitant NSAIDs to reduce gastrointestinal bleed risk. This approach aligns with ACC/AHA guideline recommendations.
Samantha Leong
8 Sep 2025
Just a friendly reminder to keep an eye on your lab work: CBC, BMP, and liver enzymes every three to six months are vital, especially if your weight or kidney function has shifted. If you notice unexplained bruising or nosebleeds, contact your cardiology team right away – early detection can prevent serious complications. Also, try to maintain consistent timing for your doses; breakfast and dinner work well for most people. Finally, keep a written list of all medications, even over‑the‑counter ones, to share with your pharmacist.
Taylor Van Wie
12 Sep 2025
Our nation’s health care system should prioritize evidence‑based therapies, and apixaban is a prime example. The data show lower bleeding rates than warfarin, which means fewer hospital stays for Americans. Do not let outdated myths about “blood thinners” deter you. Stick to the guideline‑driven dosing and you’ll stay safe.
carlee Lee
17 Sep 2025
Check kidney function before each dose change. Stay on the schedule.
chuck thomas
22 Sep 2025
Imagine your medication routine as a well‑orchestrated symphony; each dose is a note that must hit at the right moment. Skipping a beat throws the whole piece off‑balance, just like missing a dose can tip the clot‑bleed equilibrium. Pair your apixaban schedule with daily habits-maybe brushing teeth or your morning coffee-to make it effortless. And remember, the “missed dose” rule isn’t an excuse to double up; take it as soon as you recall, then continue as normal.
Gareth Pugh
26 Sep 2025
Apixaban’s twice‑daily cadence keeps plasma levels steady-no peaks, no valleys. It’s a smooth ride compared to the roller‑coaster of warfarin’s INR swings. Keep your meds handy on the nightstand, and you’ll never miss a beat.
Illiana Durbin
1 Oct 2025
Stay mindful of dehydration, especially when diuretics are cranked up. Low fluid can concentrate the drug and raise bleed risk. A simple tip: track your daily weight; sudden jumps may signal fluid shifts that need a lab check.
Tyler Heafner
6 Oct 2025
For patients with concurrent heart failure and atrial fibrillation, adherence to the prescribed apixaban regimen is paramount. Do not alter the dosage without consulting your cardiologist, even if you feel well. Routine laboratory monitoring should include renal function and complete blood count. If you are scheduled for any invasive procedure, obtain a written peri‑operative plan from your care team to avoid unnecessary interruptions.
anshu vijaywergiya
10 Oct 2025
Let’s celebrate the fact that apixaban spares us from the endless INR trips – a true blessing for anyone juggling heart failure meds. The drug’s lack of food interactions means you can finally eat your leafy greens without fear. Remember, though, that strong CYP3A4 inhibitors can raise its levels, so always double‑check new prescriptions. And when you’re on a road trip, keep a spare bottle in your carry‑on; airports love to confiscate liquids, but prescription meds are an exception.
ADam Hargrave
15 Oct 2025
Oh sure, because we all love reading drug monographs while waiting for the bus. Apixaban is “better” than warfarin-yeah, it has a fancy name and fewer lab visits, but it’s still a blood thinner, not a magic wand. If you ignore drug‑drug interactions, you might end up with a bleed that’s more dramatic than any Reddit drama thread. So, skip the sarcasm, read the label, and keep those pills where they belong.
Michael Daun
19 Oct 2025
apixaban works well for af and dvt. watch kidney fn. avoid nsaids.
keep a schedule. refill early.
Rohit Poroli
24 Oct 2025
From a pharmacokinetic standpoint, apixaban exhibits a predictable exposure profile, rendering routine coagulation monitoring obsolete. However, in patients with fluctuating creatinine clearance due to advanced heart failure, therapeutic drug monitoring may become clinically relevant. Integration of decision‑support tools within electronic health records can flag potential drug‑drug interactions, especially with potent P‑gp inhibitors such as ketoconazole. Moreover, multidisciplinary coordination between cardiology, nephrology, and oncology is essential when managing cancer‑associated thrombosis on a DOAC regimen. Lastly, educate patients on recognizing early hemorrhagic signs to facilitate prompt intervention.
William Goodwin
29 Oct 2025
💡 Quick tip: set two daily alarms on your phone-one for morning, one for night-to keep that twice‑daily rhythm alive! 😄 If you’re traveling across time zones, adjust the second alarm by an hour, not both, to maintain roughly 12‑hour spacing. Remember, you can crush apixaban tablets if you have dysphagia, but always confirm with your pharmacy first. And hey, a gentle reminder that you don’t need to avoid your favorite leafy greens-they’re perfectly fine with apixaban. Stay safe, stay steady, and keep those meds where you can see them! 🌟
Isha Bansal
2 Nov 2025
When considering apixaban for a patient with heart failure, one must first evaluate the underlying indication: atrial fibrillation, venous thromboembolism, or left‑ventricular thrombus. If atrial fibrillation is present, the CHA₂DS₂‑VASc score becomes the primary tool to gauge stroke risk, awarding one point for heart failure itself and influencing the threshold for anticoagulation. In the case of venous thromboembolism, the decision to opt for a DOAC over warfarin should incorporate factors such as renal function, potential drug interactions, and patient adherence capabilities. For left‑ventricular thrombus, while warfarin has historically been the mainstay, emerging observational data suggest that apixaban may be an acceptable alternative, especially when frequent INR monitoring is impractical; however, this off‑label use demands a shared decision‑making process. Renal function assessment is pivotal, as the drug’s clearance is partially dependent on creatinine clearance; patients with a CrCl below 30 mL/min may require dose reduction or an alternative agent. Moreover, clinicians must be vigilant about concomitant medications that are strong P‑glycoprotein or CYP3A4 inhibitors or inducers, noting that agents such as ketoconazole may increase apixaban exposure and thus bleeding risk, whereas rifampin can lower it, potentially predisposing to thrombotic events. Bleeding risk assessment should not be overlooked-tools like HAS‑BLED can be employed, but clinical judgment remains essential, particularly in the frail elderly, who may have an elevated propensity for intracranial or gastrointestinal hemorrhage. The timing of dose interruption prior to invasive procedures hinges upon the bleeding risk of the procedure and the patient’s renal function; a low‑risk dental cleaning may only require a 24‑hour hold, while major orthopedic surgery might necessitate a 48‑ to 72‑hour discontinuation. Bridging with heparin is generally unnecessary for DOACs due to their rapid onset and offset, yet individual patient circumstances may dictate otherwise. Post‑procedure, the re‑initiation of apixaban should be individualized, balancing hemostasis with thrombosis prevention, typically within 24 hours for low‑risk and 48–72 hours for high‑risk surgeries. Patient education is a cornerstone: informing patients to recognize signs of major bleeding such as melena, hematuria, or neurologic changes, and to seek immediate medical attention can greatly mitigate adverse outcomes. Furthermore, advising patients to avoid concomitant use of NSAIDs and to limit alcohol consumption can reduce incremental bleeding risk. In the broader context, adherence support tools-pill boxes, medication apps, and caregiver involvement-have demonstrated efficacy in maintaining consistent therapeutic levels, thereby reducing both thrombotetric and hemorrhagic complications. Finally, regular follow‑up visits, at least every six months, should include a comprehensive review of renal function, medication changes, and any bleeding or clotting events to dynamically adjust therapy as the patient’s clinical status evolves.
Ken Elelegwu
7 Nov 2025
One must not overlook the epistemological ramifications of prescribing a direct oral anticoagulant without a rigorous appraisal of the patient’s hemostatic milieu. The pervasive reliance on randomized controlled trial data, while laudable, may obfuscate nuanced patient‑specific variables such as subclinical hepatic insufficiency or borderline renal impairment, which subtly shift the therapeutic window. In the grand tapestry of cardiovascular therapeutics, apixaban occupies a privileged niche, yet its application should be tempered by a dialectical inquiry into alternative antithrombotic strategies. I encourage colleagues to engage in a meticulous audit of prescribing patterns, thereby fostering a culture of reflective practice rather than mere algorithmic compliance. Let us, therefore, elevate the discourse beyond rote guideline adherence to a more sophisticated, patient‑centered deliberation.
Gene Nilsson
12 Nov 2025
Adherence to prescribed dosage is essential.
Vintage Ireland
16 Nov 2025
Interesting point about the importance of timing; I actually set my alarm for both doses and it’s saved me from missed pills. Also, I’ve found that a brief note on the fridge helps remind me to check my kidney labs before the next refill.
Anshul Gupta
21 Nov 2025
While the emojis are cute, the real issue is that many patients ignore drug‑drug interactions until a bleed occurs. The post could have stressed the need for a pharmacist review when starting new antibiotics. Also, beware of over‑reliance on patient‑initiated misses; clinicians should provide clear instructions for dose‑holding.