Heart Arrhythmias from Medications: Warning Signs and How to Manage Them
Medication Arrhythmia Risk Calculator
Assess Your Risk
This tool estimates your risk of medication-induced arrhythmias based on key factors identified in medical research.
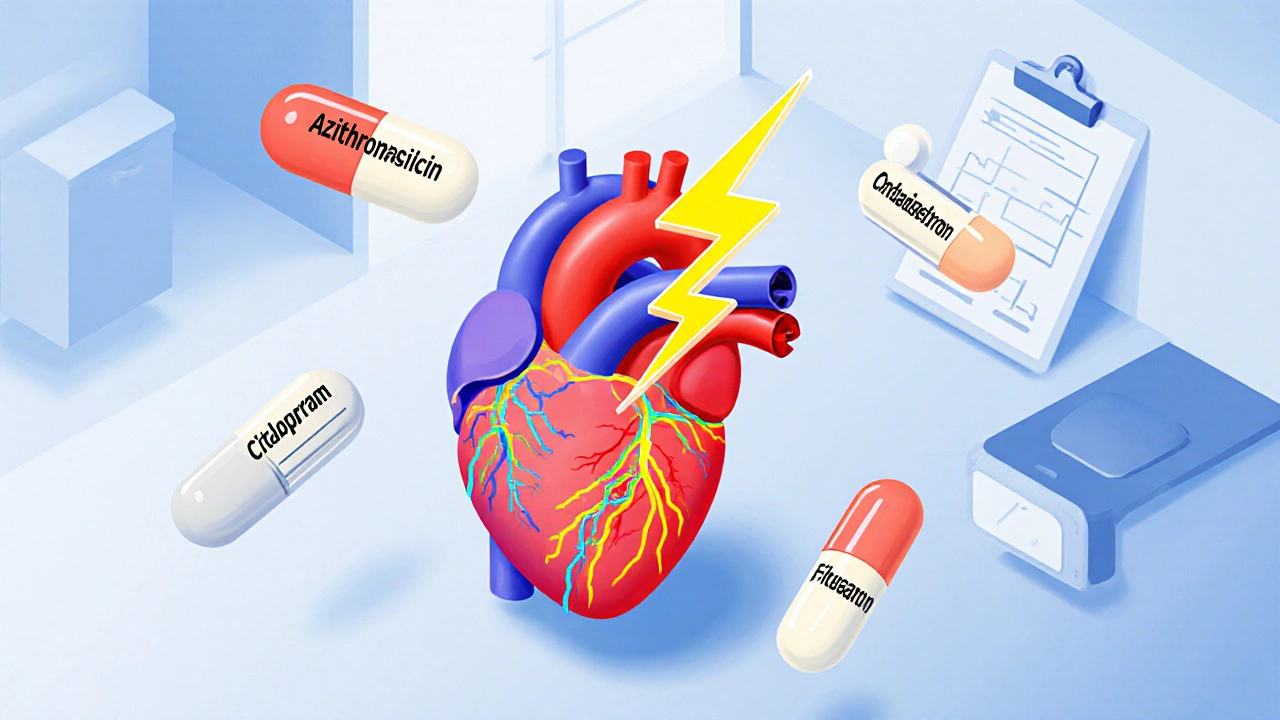
More than 400 common medications can trigger dangerous heart rhythm problems - and many people don’t realize it until it’s too late. From antibiotics to antidepressants, even drugs meant to treat heart conditions can accidentally cause life-threatening arrhythmias. If you’re taking any prescription or over-the-counter medicine and suddenly feel your heart racing, fluttering, or skipping beats, it might not be stress or caffeine. It could be your medication.
What Exactly Is a Drug-Induced Arrhythmia?
A drug-induced arrhythmia is an abnormal heartbeat caused by a medication. It doesn’t mean your heart is broken - it means something you’re taking is interfering with the electrical signals that keep your heart beating regularly. These disruptions can cause everything from mild palpitations to sudden cardiac arrest. The most common type is QT prolongation, where the heart takes longer than normal to recharge between beats. This delay can trigger a dangerous rhythm called torsades de pointes, which can lead to fainting, seizures, or death if not treated quickly. Over 25 medications now carry FDA black box warnings for this exact risk, and new ones are added every year. Some of the most frequent culprits include:- Antibiotics like azithromycin and levofloxacin
- Antidepressants such as citalopram and escitalopram
- Antipsychotics like haloperidol and ziprasidone
- Anti-nausea drugs like ondansetron
- Even heart medications like amiodarone and flecainide - yes, drugs meant to fix arrhythmias can cause them
Who’s at Highest Risk?
Not everyone who takes these drugs will have problems. But certain factors make arrhythmias much more likely:- Age 65+: Over 60% of severe cases happen in older adults. Their kidneys and liver don’t clear drugs as efficiently, so levels build up.
- Low potassium or magnesium: These minerals help your heart’s electrical system work right. If you’re on diuretics (water pills), have poor diet, or are dehydrated, your levels can drop dangerously low.
- Multiple QT-prolonging drugs: Taking two or more drugs that stretch the QT interval increases your risk by 300-500%. A common example? An antibiotic plus an antidepressant.
- Excessive alcohol: More than three drinks a day triples your risk.
- Genetics: About 15% of people of African ancestry and 12% of East Asian ancestry carry gene variants that make them far more sensitive to these drugs.
Warning Signs You Can’t Ignore
Most people don’t feel anything until it’s serious. But early signs are there - if you know what to look for:- Palpitations: A fluttering, pounding, or irregular heartbeat - reported by 70-80% of patients before a serious event.
- Dizziness or lightheadedness: Especially when standing up. This isn’t just ‘getting old’ - it’s your heart not pumping enough blood.
- Fatigue or weakness: If you’re suddenly exhausted after minimal activity, your heart might be struggling.
- Chest discomfort: Not always sharp pain. Sometimes it’s pressure, tightness, or just a strange feeling.
- Fainting or near-fainting: This is a red flag. If you’ve passed out or felt like you might, get checked immediately.

How Doctors Diagnose It
The first test is always an ECG - a simple, painless scan of your heart’s electrical activity. If your QT interval is longer than 450 milliseconds in men or 460 in women, that’s a warning sign. But ECGs aren’t always enough. Doctors will also check:- Blood levels: Potassium, magnesium, calcium - all need to be in the safe range. Target: potassium above 4.0 mEq/L, magnesium above 2.0 mg/dL.
- Drug levels: For medications like digoxin, even a small overdose can cause arrhythmias. Normal levels are 0.5-2.0 ng/mL. Above 2.0? High risk.
- Medication review: Every pill you take - including supplements like licorice root or St. John’s wort - gets looked at. Many herbal products also prolong QT.
What Happens Next? Management Strategies
The good news? In 75-85% of cases, stopping or adjusting the drug fixes the problem. Here’s how it usually works:- Stop or switch the medication: If possible, your doctor will replace the risky drug with a safer alternative. For example, switching from azithromycin to amoxicillin for an infection.
- Correct electrolytes: If your potassium or magnesium is low, you’ll get supplements - sometimes IV in the hospital.
- Monitor closely: A repeat ECG within 72 hours of starting a new high-risk drug is standard practice. Some patients need weekly checks.
- Reduce other triggers: Cut back on caffeine, alcohol, and smoking. Caffeine alone causes palpitations in 25-30% of patients, though it rarely triggers serious arrhythmias by itself.
- Consider a pacemaker: For patients with severe bradycardia from beta-blockers (like metoprolol), dose reduction helps 60-70% of the time. But if symptoms persist, a pacemaker may be needed to keep the heart safe while still controlling atrial fibrillation.
- Advanced treatments: Only 5-10% need catheter ablation. Less than 2% require surgery.

What You Can Do Right Now
You don’t have to wait for a crisis. Here’s how to protect yourself:- Ask your doctor: ‘Could this medicine affect my heart rhythm?’ before starting any new prescription or OTC drug.
- Keep a medication list: Include every pill, patch, supplement, and herbal remedy. Bring it to every appointment.
- Get a baseline ECG: Especially if you’re over 60, have kidney disease, or are on multiple meds.
- Check your electrolytes: Ask for a simple blood test if you’re on diuretics or have been vomiting or sweating a lot.
- Know your family history: If close relatives had sudden cardiac arrest or unexplained fainting, tell your doctor.
The Future: Personalized Medicine Is Coming
Researchers are now testing genetic screening before prescribing high-risk drugs. Studies using CRISPR-edited heart cells show that people with certain gene variants (like S1103Y and R1193Q) are far more likely to have dangerous reactions. In the next few years, doctors may run a quick DNA test before prescribing antibiotics or antidepressants to high-risk patients. The American College of Cardiology is rolling out a decision tool in 2024 that calculates your personal arrhythmia risk based on age, meds, electrolytes, and genetics. This could cut severe cases by 30-40% in five years.Final Thought: Don’t Assume It’s ‘Just a Side Effect’
Heart arrhythmias from medications are not rare. They cause 100,000-150,000 hospitalizations in the U.S. every year and cost over $1.2 billion. But nearly two-thirds of severe cases could be prevented with better awareness. If you’re taking medication and feel off - really off - trust your body. Don’t brush it off. Talk to your doctor. Ask for an ECG. Get your levels checked. You might just save your life.Can over-the-counter drugs cause heart arrhythmias?
Yes. Common OTC drugs like pseudoephedrine (in cold medicines), antihistamines like diphenhydramine (Benadryl), and even some herbal supplements like licorice root or ephedra can prolong the QT interval and trigger arrhythmias. Always check with your pharmacist before taking new OTC meds, especially if you’re already on heart or psychiatric medications.
How long does it take for a drug to cause an arrhythmia?
It can happen quickly - within hours or days. For antibiotics like azithromycin, the highest risk is in the first 7 days of use. For drugs like amiodarone, arrhythmias may develop after months or even years of use. That’s why ongoing monitoring matters, even if you’ve been on a medication for a while.
Is it safe to stop a medication if I suspect it’s causing arrhythmias?
Never stop a prescribed medication without talking to your doctor first. Stopping suddenly can be dangerous - for example, stopping a beta-blocker too fast can cause rebound high blood pressure or even a heart attack. Instead, call your doctor, describe your symptoms, and ask for guidance. They may recommend a temporary switch or a test to confirm the cause.
Can caffeine or alcohol trigger arrhythmias from medications?
Yes. Caffeine can worsen palpitations and make arrhythmias feel worse, though it rarely causes serious rhythm problems alone. Alcohol is far more dangerous - especially in large amounts. More than three drinks a day triples your risk of drug-induced arrhythmias. If you’re on a QT-prolonging drug, it’s best to avoid alcohol entirely.
Are there any medications that are completely safe for people with heart rhythm issues?
There’s no universal ‘safe’ list - it depends on your individual risk. But some drugs have lower arrhythmia risk. For example, penicillin-based antibiotics are safer than macrolides. Sertraline is often preferred over citalopram for depression. Your doctor can use updated risk tools to pick the safest option for your profile.
Should I get genetic testing for drug-induced arrhythmias?
Not routinely - yet. But if you’ve had a drug-induced arrhythmia, unexplained fainting, or a family history of sudden cardiac death, genetic testing may be worthwhile. Research is advancing fast, and in the next few years, this may become standard before prescribing high-risk drugs.






Comments (8)
Lashonda Rene
4 Nov 2025
i just found out my grandma got hospitalized last year because she was on azithromycin and citalopram together and no one told her it could mess with her heart. she’s 72 and has always been healthy but suddenly started fainting after her cold got worse. the doctor said it was QT prolongation and she almost died. i’m crying just thinking about it. why isn’t this common knowledge? like, every pharmacy should have a sign when you pick up these meds. i’ve been checking every pill i take now, even the ones from the dollar store. my mom thinks i’m paranoid but i’d rather be annoying than dead.
Andy Slack
4 Nov 2025
THIS. I’ve been on amiodarone for 3 years and never knew it could cause the very thing it’s supposed to fix. My cardiologist never mentioned it. I thought my occasional dizziness was just aging. Turns out my potassium was at 3.1. I started eating bananas like they’re going out of style and my heart stopped feeling like it was doing backflips. Don’t ignore the little signs. Your body talks. You just gotta listen.
Rashmi Mohapatra
6 Nov 2025
so many people in india take antibiotics without prescription and then wonder why they get dizzy or their heart races. my cousin took levofloxacin for a sore throat and passed out at the market. no ekg, no blood test, just a doctor saying 'maybe stress'. dumb. if you're on more than 2 pills, ask for a QT check. it's 5 minutes and free in gov hospitals. why wait till you're in ICU?
Kelsey Veg
6 Nov 2025
let me be the one to say it: this post is 90% fearmongering. yes, some drugs can cause arrhythmias, but 99% of people won't ever have an issue. you're scaring people into thinking every antibiotic is a death sentence. if you're healthy, active, and not on 7 meds, you're fine. stop reading doom scrolls and go for a walk. your anxiety is probably what's making your heart flutter.
Alex Harrison
8 Nov 2025
my doc just switched me from citalopram to sertraline after i mentioned my palpitations. i didn’t even connect it until i read this. i’ve been on it for 2 years and thought it was just my coffee habit. i got my ekg and potassium checked and turns out i was low as hell. i’m taking magnesium now and feel 100% better. thanks for the heads up. i’m printing this out for my mom too-she’s on ondansetron and diuretics. she’s gonna hate me for it but i don’t care.
Jay Wallace
8 Nov 2025
Oh, so now we’re blaming Big Pharma for people not reading the tiny print? Get a grip. If you can’t read a medication label or ask your doctor a simple question, maybe you shouldn’t be allowed to take pills. This country is turning into a lawsuit-happy, hypochondriac circus. I take 8 meds and I’ve never had an issue. Stop making people paranoid. Your body isn’t a fragile porcelain doll.
Alyssa Fisher
8 Nov 2025
What’s fascinating here isn’t just the drug interactions-it’s how medicine still treats the heart like a black box. We test drugs for toxicity, but rarely for how they disrupt the heart’s subtle bioelectrical symphony. We’ve got the tech to map ion channels, to screen for genetic vulnerabilities like S1103Y-but we don’t do it because it’s expensive, not because it’s unnecessary. The real tragedy isn’t the arrhythmias-it’s that we wait for someone to collapse before we ask: ‘Why didn’t we look deeper?’
Alyssa Salazar
8 Nov 2025
Let’s be real-this is why precision medicine is the future. You’ve got pharmacogenomics, EHRs, AI-driven risk calculators… yet we’re still giving people amiodarone like it’s aspirin. The fact that we don’t routinely screen for QT risk before prescribing is a systemic failure. And yes, I’m calling it out: if your provider hasn’t mentioned electrolytes or genetic risk factors, they’re practicing 20th-century medicine. Get a second opinion. Demand the ECG. Your life isn’t a gamble.