When to Monitor Anti-Xa Levels for LMWH: Signs That Demand Testing

LMWH Anti-Xa Testing Decision Tool
Is Anti-Xa Testing Needed?
This tool helps determine if anti-Xa testing is clinically indicated based on evidence-based guidelines from the article.
Most people on low molecular weight heparin (LMWH) like enoxaparin or dalteparin never need their anti-Xa levels checked. That’s because these drugs are designed to work reliably with fixed doses-no lab tests required. But when things go wrong-when a patient bleeds for no reason, or a clot forms despite treatment-that’s when anti-Xa monitoring becomes critical. It’s not about routine checks. It’s about anti-Xa monitoring as a safety net for high-risk situations where the body isn’t responding as expected.
Why Anti-Xa Monitoring Isn’t Routine
LMWH works by blocking factor Xa, a key player in blood clotting. Unlike unfractionated heparin, which needs frequent aPTT checks, LMWH has a predictable dose-response in most people. Studies show that in healthy adults, standard doses of enoxaparin 40 mg daily or 1 mg/kg twice daily reliably keep anti-Xa levels in the therapeutic range. That’s why major guidelines, including the 2021 American College of Chest Physicians update, strongly advise against routine monitoring. In fact, a 2015 analysis of over 12,800 patients found no difference in outcomes between those monitored and those not. Yet, in 2023, a hospital audit in Ventura County found that nearly 72% of anti-Xa tests ordered were unnecessary. Many were done after surgery just to “check,” or because a nurse saw a high INR and assumed it was related. That’s dangerous. Unnecessary testing leads to unnecessary dose changes-and those changes can cause bleeding.When You Absolutely Need to Check Anti-Xa Levels
There are only a few clear, evidence-backed reasons to draw an anti-Xa level. These aren’t theoretical-they’re real clinical red flags.- Major bleeding without trauma: If a patient on LMWH suddenly develops a large hematoma, gastrointestinal bleed, or intracranial hemorrhage with no obvious cause, their anti-Xa level may be supratherapeutic. This is especially true in patients with kidney problems.
- Thrombosis on therapeutic dosing: If someone gets a deep vein thrombosis or pulmonary embolism while on a full therapeutic dose of enoxaparin, their anti-Xa level might be too low. This happens more often in obese patients or those with renal impairment.
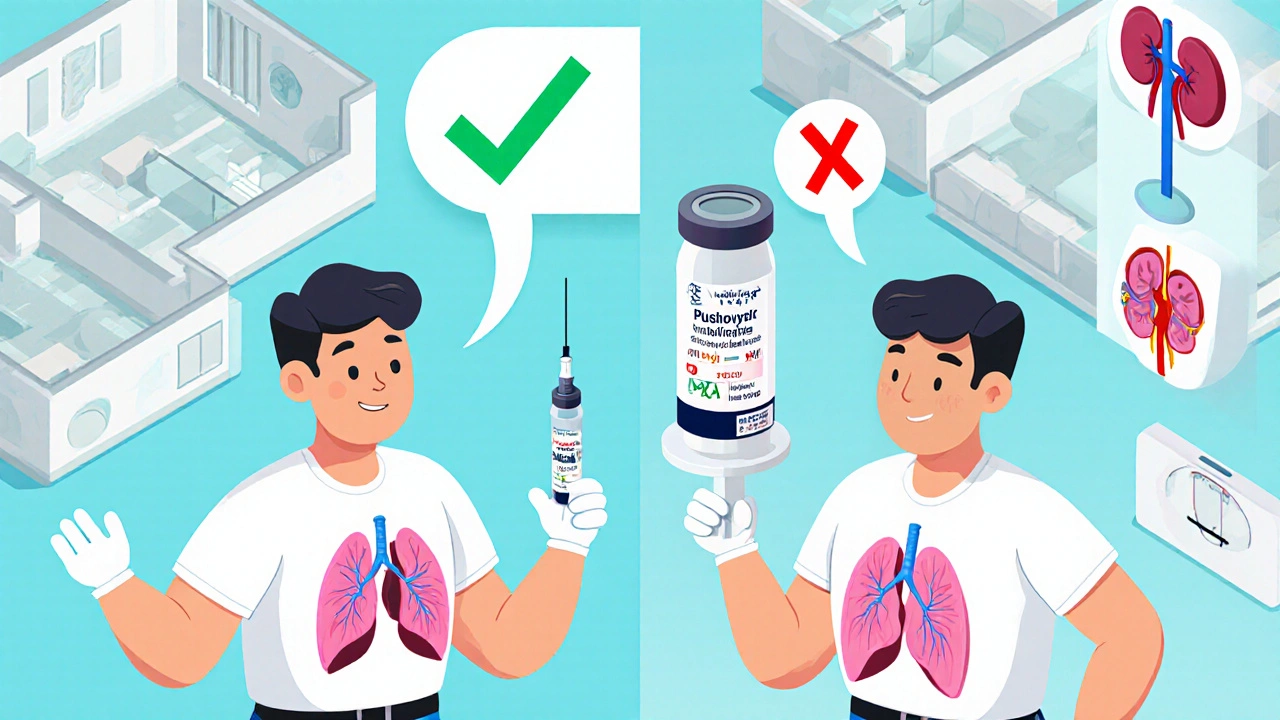
- Severe kidney impairment: When creatinine clearance drops below 30 mL/min, LMWH builds up. At CrCl under 15 mL/min, half-life jumps from 4-5 hours to over 12 hours. A single dose can linger dangerously long. Anti-Xa testing here isn’t optional-it’s life-saving.
- Extreme body weight: Patients under 40 kg or over 150 kg don’t fit standard dosing formulas. A 320 kg trauma patient on enoxaparin 40 mg daily might be grossly underdosed. Anti-Xa levels can confirm whether the dose needs to be adjusted based on total body weight.
- Pregnancy: During pregnancy, volume of distribution increases, and renal clearance rises. The target anti-Xa range shifts to 0.2-0.6 IU/mL for therapeutic dosing, lower than in non-pregnant adults. Monitoring ensures both mother and baby are protected.
- Suspected heparin-induced thrombocytopenia (HIT): If platelets drop sharply on LMWH, and you need to switch to another anticoagulant like argatroban, anti-Xa levels help guide the transition to ensure no gap in protection.
How and When to Draw the Test
Timing matters. Drawing an anti-Xa level at the wrong time gives you useless data. For therapeutic dosing, the sample must be drawn 4-6 hours after the injection-that’s when the peak level occurs. This reflects the maximum anticoagulant effect. Trough levels (just before the next dose) are rarely used for LMWH because they don’t correlate well with clinical outcomes. The test shouldn’t be done before the third dose. It takes at least two full cycles for the drug to reach steady state. If you test too early, you’re just measuring drug accumulation, not true pharmacodynamics. Most hospital labs use STA-R Evolution or ACL TOP analyzers. Turnaround time is usually 2-4 hours. But here’s the catch: results vary between labs. Inter-lab variation can be as high as 15%. That means a level of 0.8 IU/mL at one hospital might read 0.9 at another. Always know your lab’s reference range.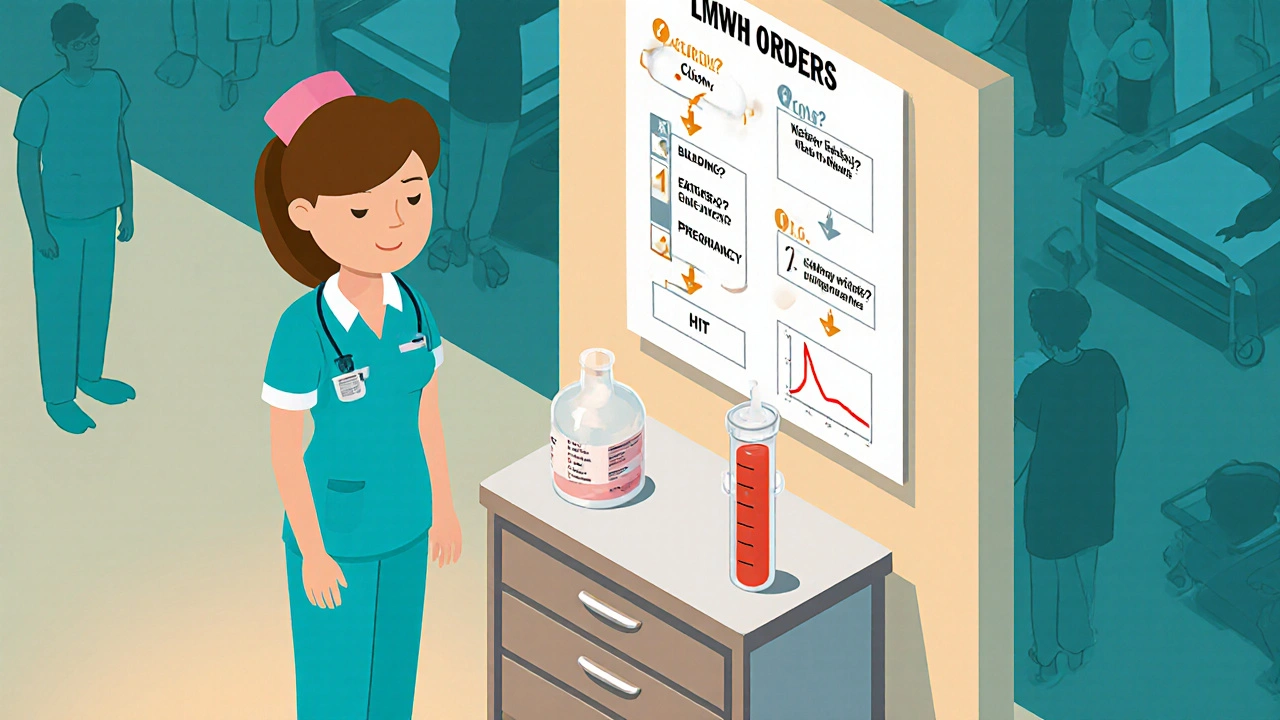
Therapeutic Ranges: What Numbers Mean
Anti-Xa levels aren’t one-size-fits-all. The target depends entirely on why you’re giving the drug.- Prophylactic dosing (e.g., after surgery or for immobility): 0.2-0.5 IU/mL
- Therapeutic dosing (e.g., for DVT or PE): 0.6-1.0 IU/mL
- Pregnancy (therapeutic): 0.2-0.6 IU/mL
What Anti-Xa Testing Can’t Do
It’s easy to overestimate what this test can tell you. Here’s what it doesn’t do:- It doesn’t predict bleeding risk in standard populations. A patient with an anti-Xa level of 0.9 IU/mL might be fine, while another with 0.7 IU/mL might bleed-because of age, liver disease, or concomitant medications.
- It can’t distinguish between different LMWHs. Enoxaparin and dalteparin both inhibit factor Xa, but they’re chemically different. The test just measures total anti-Xa activity.
- It won’t detect direct oral anticoagulants (DOACs) like apixaban or rivaroxaban. If someone’s on both LMWH and a DOAC, the anti-Xa level will be falsely elevated.
- It doesn’t replace clinical judgment. A single high level without bleeding? Don’t rush to reduce the dose. Look at the whole picture: blood pressure, hemoglobin trend, recent trauma, other drugs.
Real Cases: What Works in Practice
One patient, a 68-year-old woman with kidney failure (CrCl 18 mL/min), was on enoxaparin 40 mg daily after a hip replacement. Two days later, she developed a large thigh hematoma. Her anti-Xa level came back at 1.8 IU/mL-way above therapeutic. The dose was held, and she was switched to a non-renal cleared agent. She recovered without further bleeding. Another case: a 320 kg man after a motor vehicle crash. He was on enoxaparin 40 mg daily-standard prophylactic dose. He developed a pulmonary embolism on day three. His anti-Xa level was 0.1 IU/mL. He was re-dosed based on total body weight, and his level rose to 0.4 IU/mL. No further clots. These aren’t rare. In a 2018 audit, 92% of appropriate anti-Xa tests led to correct dose changes-and no complications followed those adjustments. But 8% of inappropriate adjustments caused bleeding.How to Avoid Mistakes
The biggest problem isn’t the test-it’s the order. Too many providers order anti-Xa levels out of habit, fear, or confusion. Here’s how to fix it:- Use order sets: Hospitals like Vanderbilt implemented pharmacist-led electronic order sets that only allow anti-Xa testing if one of the six clinical triggers is selected.
- Train staff: Nurses and residents need to know when to ask for the test. A simple flowchart posted in nursing stations helps: “Bleeding? Clot? Kidney failure? Extreme weight? Pregnancy? HIT?” If none, don’t order.
- Don’t rely on single values: One high level doesn’t mean overdose. Look at trends. Did hemoglobin drop? Is the patient swollen? Is the dose correct for their weight and kidney function?
- Know your lab’s range: Always check the reference range printed on the report. Don’t assume it’s the same as your textbook.
The Bottom Line
Anti-Xa monitoring for LMWH isn’t about precision medicine for everyone. It’s about targeted safety for the few who need it. Most people on enoxaparin will never need this test. But for those with kidney failure, extreme weight, pregnancy, or unexpected complications-it can prevent death. The goal isn’t to test more. It’s to test smarter. When bleeding happens, when clots form despite treatment, when the body’s chemistry changes-then, and only then, check the anti-Xa level. That’s how you turn a lab test from a waste of money into a lifesaving tool.Do I need to check anti-Xa levels every time someone is on LMWH?
No. Routine anti-Xa monitoring is not recommended for most patients. LMWH is designed to work reliably with fixed doses in people with normal kidney function and average body weight. Testing is only needed when there’s a clinical red flag-like unexpected bleeding, a clot forming despite treatment, severe kidney disease, extreme body weight, or pregnancy.
What’s the right time to draw an anti-Xa level?
For therapeutic dosing, draw the sample 4 to 6 hours after the injection-this is when the drug reaches its peak effect. For prophylactic dosing, timing is less critical, but consistency matters. Never test before the third dose, as steady-state levels aren’t reached until then.
Can anti-Xa levels predict bleeding risk?
Not reliably in most people. A high anti-Xa level doesn’t automatically mean bleeding will happen, and a normal level doesn’t guarantee safety. The test shows drug concentration, not clinical risk. Always combine it with the patient’s symptoms, kidney function, weight, and other medications.
Is anti-Xa testing the same as aPTT?
No. aPTT is used to monitor unfractionated heparin, not LMWH. LMWH has a different mechanism-it mainly blocks factor Xa, not thrombin-so aPTT is unreliable and often normal even when LMWH is at therapeutic levels. Anti-Xa is the only accurate test for LMWH.
How much does an anti-Xa test cost?
In the U.S., the test typically costs between $45 and $75 per draw, depending on the lab and insurance. Medicare reimburses around $58 as of 2023. The real cost isn’t just the price-it’s the risk of inappropriate dose changes if the test is ordered without a clear clinical reason.
Can obesity affect LMWH dosing without testing?
Yes. For patients over 150 kg, standard dosing based on ideal body weight can lead to underdosing and clotting. Current guidelines recommend dosing based on total body weight, not ideal weight. While anti-Xa monitoring can confirm adequacy, studies show that using total body weight alone often achieves therapeutic levels without testing-unless there’s an unexpected outcome.
What happens if I adjust the dose based on a single anti-Xa level?
You might cause harm. A single elevated level without clinical signs of bleeding doesn’t mean the patient is over-anticoagulated. Many patients have isolated high levels due to lab variation, timing errors, or temporary changes in kidney function. Always correlate with symptoms, trends, and clinical context before changing the dose.





Comments (15)
Kristina Williams
17 Nov 2025
So let me get this straight - hospitals are spending thousands on tests that aren’t needed, and nurses are ordering them because they saw a high INR? That’s like calling 911 because your coffee’s cold. People are scared of doing nothing, so they do something stupid instead. 😒
Louie Amour
18 Nov 2025
Wow. This is the kind of textbook-level insight that only someone who’s never treated a real patient could write. You’re basically saying ‘don’t test unless someone’s dying’ - genius. Meanwhile, in the real world, we don’t wait for bleeding to happen before we check if the patient’s anticoagulated. You’re not a clinician. You’re a PowerPoint presenter with a medical degree.
Shilpi Tiwari
18 Nov 2025
Interesting breakdown, but you missed the pharmacokinetic nuance in renal clearance dynamics - particularly the non-linear accumulation in CrCl <15 mL/min due to reduced tubular secretion and altered protein binding. The 2018 JTH paper by Patel et al. showed a 3.2x increase in half-life in end-stage renal disease, which correlates with peak anti-Xa levels >1.5 IU/mL even at prophylactic dosing. This isn't just clinical judgment - it's pharmacodynamic imperative.
Holly Powell
18 Nov 2025
Let’s be real - this whole post reads like a corporate compliance slide deck written by someone who’s never held a syringe. The ‘six triggers’? That’s not evidence. That’s a checklist someone at the hospital admin office dreamed up to reduce liability. Meanwhile, patients are getting clots because someone was too lazy to check the level when the weight was 200 kg and the creatinine was 1.8. You don’t get to outsource clinical reasoning to an algorithm.
Emanuel Jalba
20 Nov 2025
THIS IS WHY PEOPLE DIE IN HOSPITALS 😭😭😭 I had my uncle on Lovenox after knee surgery and they didn't check his levels and he got a PE and they didn't even tell us until he was in ICU for 3 days. I'm crying right now. This is a national scandal. #MedicalMalpractice #LMWHIsNotASnack
Heidi R
22 Nov 2025
You’re wrong. You always test. Always. If you’re not testing, you’re not practicing medicine. You’re guessing. And guessing kills.
Brenda Kuter
24 Nov 2025
Who’s really behind this ‘don’t test’ agenda? Big Pharma? The labs? The hospital administrators who get bonuses for cutting ‘unnecessary tests’? Someone’s making money off this. Someone’s pushing this narrative. And it’s not the patients. It’s not the nurses. It’s not the doctors who see the bodies. It’s the suits. 💔
Shaun Barratt
25 Nov 2025
While the clinical guidelines referenced are generally sound, the assertion that anti-Xa monitoring is unnecessary in standard populations requires qualification. Variability in renal function, even within normal ranges, may influence pharmacokinetics in subpopulations not adequately represented in the cited 2015 meta-analysis. Additionally, the inter-laboratory variation cited (up to 15%) undermines the reliability of threshold-based decision-making. A standardized assay protocol and reference material are required before widespread de-implementation.
Katelyn Sykes
26 Nov 2025
Y’all are overcomplicating this. If someone’s bleeding or clotting - check the level. If they’re obese or have bad kidneys - check it. If they’re pregnant - check it. If they’re fine? Don’t. Stop turning medicine into a spreadsheet. You’re not a robot. You’re a human helping another human. Trust your gut, know your patient, and test when it matters. That’s it. 💪
Gabe Solack
27 Nov 2025
Great breakdown. I’ve seen both sides - the over-testing and the under-testing. But the real win is when you pair the lab result with the patient’s story. One guy had a level of 0.8 but was pale, hypotensive, and had a dropping Hgb - we held the dose immediately. Another had a 1.1 but was a 300-pound athlete with no bleeding - we left it alone. Numbers don’t tell the whole story. People do.
Yash Nair
27 Nov 2025
USA doctors think they know everything but in India we know how to handle LMWH better. We test every patient because we dont trust the weight formulas. Our patients are different. Our bodies are different. Why copy your flawed system? You think your guidelines are gold? LOL. We save lives by testing more.
Bailey Sheppard
28 Nov 2025
This is actually really helpful. I’ve seen so many people get confused about when to test - I’m going to print this out and put it on the unit whiteboard. Clear, evidence-based, no fluff. Thanks for writing this.
Girish Pai
29 Nov 2025
Anti-Xa testing is the only objective marker we have. The fact that American hospitals are cutting it because of cost is a disgrace. In India, we don’t wait for bleeding. We monitor. We prevent. We don’t wait for death to prove we were right. This post is a warning to every Western hospital: stop prioritizing budgets over biology.
Kristi Joy
29 Nov 2025
Thank you for writing this so clearly. I’ve been trying to explain this to my team for months. So many nurses think ‘if it’s a lab test, it must be important.’ But you’re right - it’s not about testing more. It’s about testing smarter. I’m sharing this with every new resident on my team. You’ve made a difference today.
Hal Nicholas
1 Dec 2025
It’s funny how people think they’re being ‘evidence-based’ when they’re just avoiding responsibility. If you don’t test, you can’t be blamed if someone bleeds. But if you test and adjust, and they still bleed? That’s on you. So you don’t test. That’s not medicine. That’s cowardice.