Fosamax: Practical Guide to Safe Bone Health and Osteoporosis Treatment

Imagine waking up one morning, only to find out that doing something as simple as bending to tie your shoes could put your bones at risk. That’s the reality for people living with osteoporosis, a disease that quietly eats away at your bone strength. Not many people want to talk about thinning bones, but here’s a fact: in the UK, one in two women and about one in five men over 50 will break a bone because of osteoporosis. The numbers are staggering. At the frontline of defense stands a drug called Fosamax, or as the pharmacist might call it, alendronate.
Understanding Fosamax and How It Works
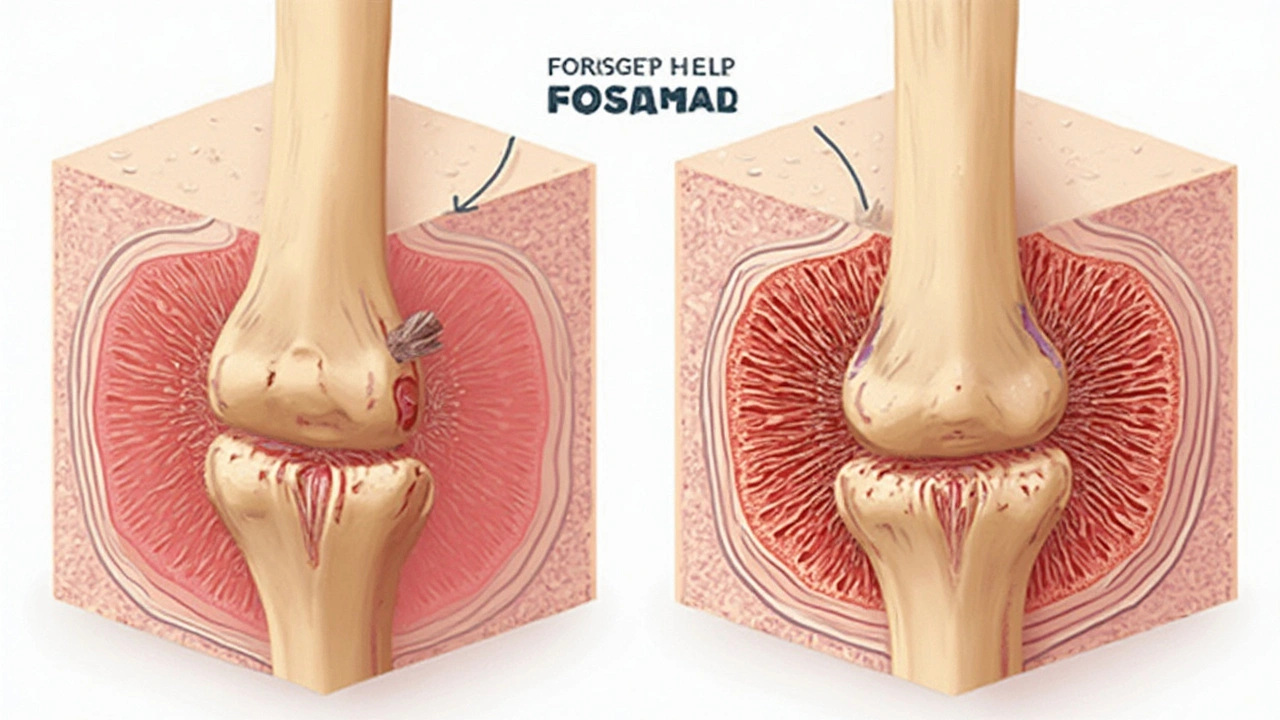
Think of your bones as a construction site, always being built up and broken down. With osteoporosis, the demolition crew works faster than the builders. Fosamax steps in to slow down that demolition. The secret? It belongs to a group of drugs called bisphosphonates. These medications latch on to your bones and put the brakes on the cells that chew up bone tissue. Over time, that means your bones can get denser and less likely to snap from life’s little slips.
The active ingredient in Fosamax, alendronate sodium, has a proven track record. First approved in the late 1990s, it’s been prescribed millions of times worldwide. In the UK, the NHS keeps it on the list of recommended treatments for postmenopausal women and older men who face high fracture risk. Not just for osteoporosis, either—Fosamax also helps in other bone-weakening conditions like Paget’s disease.
Fosamax comes in a once-weekly or daily tablet, which seems easy enough, but you can’t just pop it with your morning tea. The body doesn’t absorb it well, so timing and technique are key. Otherwise, you risk getting a prescription with no payoff.
The Realities of Taking Fosamax: What to Expect
If you’ve got Fosamax in your kitchen cupboard, you probably already know this: the instructions are a bit of a ritual. Take one tablet first thing when you wake, on an empty stomach, with a big glass of plain water. No coffee, juice, or even mineral water allowed. Then, stand or sit upright (no lounging back in bed!) for at least half an hour. Only after that can you have breakfast or even a sip of your morning brew. Sounds like a faff? There’s a reason. This careful routine helps the drug actually get into your bones and not just sit in your stomach causing trouble.
Stick to the schedule, because missing a dose can lower your protection. If you take the once-a-week pill, pick a day and make it a habit—maybe mark it on your phone’s calendar. Where people fall off the wagon is with the follow-through. Studies from UK clinics have shown that only about 50% of people are still taking their bisphosphonate prescription one year later. Life gets busy, routines slip, and side effects pop up.
| Group | Continuation Rate |
|---|---|
| Women (over 50) | 53% |
| Men (over 50) | 48% |
| All Patients (Average) | 50% |
But the upside? After a year or so of regular use, bone density scans almost always show improvement. That means fewer broken wrists, hips, and vertebrae, which for many people means a longer, more independent life.
Fosamax: Side Effects, Myths, and the Facts
Every medicine has downsides, right? Fosamax is no different—talk to anyone who’s taken it long enough, and you’ll hear the stories. The most common gripe? Stomach upset. That’s why the rule about standing or sitting upright for at least 30 minutes after taking the tablet matters so much. If the pill gets stuck, it can irritate your food pipe (esophagus) and even cause ulcers. Some people find they get acid reflux for the first few weeks. If you’re unlucky, you might also notice joint or muscle pain, but it tends to ease with time. Nausea and mild headaches happen sometimes, too.
Now for the scary stuff you might have heard about online: jawbone problems and unusual thigh fractures. The official term for the jaw issue is osteonecrosis. It’s rare, mainly seen in people who take very high doses for cancer, but the risk goes up if you have dental surgery during treatment. As for the thigh fractures, it’s confusing—while Fosamax prevents most typical bone breaks, a tiny number of people might get a specific type of fracture after long-term use. Most doctors now say a “drug holiday”—taking a break after, say, five years—can help balance risk and benefit. Always talk to your healthcare team before stopping, though.
Myth-busting time: Fosamax isn’t a calcium supplement, and popping it with milk or vitamins isn’t helpful. Also, the "bone pain" you hear about isn’t common, and most side effects clear up within weeks. If anything feels wrong, let your doctor know. They’d much rather tweak your dose than hear about a hospital admission from a broken hip.
Maximizing the Benefits of Fosamax
Want to get the most from your Fosamax? Start with the basics: follow the dosing instructions to the letter. Not a morning person? Set a special alarm or leave your pills on your mobile charger—you’ll see them as soon as you wake up. Pairing it with a routine (like brushing your teeth) helps cement the habit.
Add in the unsung hero: calcium and vitamin D. Fosamax works way better if your body isn’t starved for the building blocks of bone. About 800 to 1,000 IU of vitamin D and 1,000 to 1,200 mg of calcium daily is standard in the UK. If you’re not keen on supplements, you can bump up your intake with leafy greens, dairy, fortified cereals, and soaking up a little sunlight when the Sheffield weather allows. Don’t forget weight-bearing exercise—walking, light jogging, and even garden work all help your bones stay strong.
Your dentist needs to know you’re taking Fosamax, especially before any fillings or extractions. Some folks skip this and regret it later, so make a note when filling out those medical forms. And let your doctor know if you have swallowing troubles or any history of stomach ulcers—other medicines might suit you better.
Monitor your progress with annual bone density scans. They don’t hurt—just a quick lie-down while a scanner whirs above you. Most people taking Fosamax see a steady rise in their bone density scores over two or three years, translating to real-world benefits: fewer fractures, more mobile years, and peace of mind.

Everyday Life and Conversations Around Fosamax
Talking about your meds isn’t the most exciting part of catching up with mates, but having osteoporosis (or being at risk) is more common than it seems. In local Sheffield community groups, it’s not unusual to find several folks on Fosamax comparing routines and sharing tips. Some trade recipes for calcium-rich foods; others chat about yoga classes to boost balance and cut falls.
Don’t hesitate to ask your GP or pharmacist about side effects, especially if your symptoms are affecting your mood or daily routines. If you need extra support, charities like the Royal Osteoporosis Society offer hotlines, booklets, and even peer groups where you can swap real stories (not just textbook answers).
Treating osteoporosis doesn’t end with a prescription. Simple things—grippy shoes, stair rails, brighter lights—can make your home less of a hazard. A healthy dose of realistic optimism helps, too. Your bones aren’t just scaffolding; they hold your whole story together. The science behind Fosamax is solid, but it’s the little daily choices that really add up.
If you’re weighing up Fosamax or already taking it, remember it’s a tool—one that works best with a strong game plan. Whether you’re in Sheffield or somewhere sunnier, keeping your skeleton strong is about more than just medicine. It’s about taking the right steps, every single day, to keep yourself moving and thriving for as long as possible.






Comments (12)
Kevin Galligan
14 Jun 2025
Wow, reading this feels like a masterclass in bone‑building bureaucracy – who knew a tiny tablet could demand a full‑blown morning ritual? 😏 Grab that glass of water, stand like a statue for thirty minutes, and you’ve basically earned a gold star in pharmaceutical obedience. If you can survive the ritual, your bones will thank you, and you’ll finally have an excuse to skip that extra coffee. Cheers to staying upright, literally! 😊
Dileep Jha
28 Jun 2025
While the article paints Fosamax as a panacea, one must scrutinize the pharmacodynamics beyond the hype. The drug’s affinity for hydroxyapatite crystals is indeed high, yet the resultant suppression of osteoclastic resorption can precipitate a paradoxical remodeling deficit, culminating in atypical femoral stress fractures – a classic case of over‑inhibition in bone turnover. Moreover, the reliance on patient adherence glosses over the biochemical heterogeneity inherent in bisphosphonate metabolism. In short, the mechanistic narrative is far more nuanced than a simplistic “brakes on demolition crew” analogy suggests.
Michael Dennis
13 Jul 2025
Admittedly, the guide is thorough, yet it overlooks several practical considerations. For instance, the recommendation to pair Fosamax with calcium and vitamin D lacks specificity regarding optimal serum levels, which are critical for efficacy. Additionally, the discussion of drug holidays is cursory; the criteria for initiating a holiday are not merely temporal but also based on bone turnover markers. While well‑intentioned, the article could benefit from a more rigorous examination of these clinical subtleties.
Blair Robertshaw
27 Jul 2025
yeah but the real issue is ppl just dont read the fine print and end up with esophagus irritation – thats what i see in the clinic all the time. the guide makes it sound like a walk in the park but honestly most folks cant keep a 30min upright stance without brekin their back. also the side effect stats are sus, they dont mention the rare but scary jaw necrosis case which freaks people out.
Alec Maley
11 Aug 2025
Reading this, I feel a wave of optimism for anyone tackling osteoporosis. The routine may seem fussy, but think of it as a daily act of self‑care, like brushing your teeth. Pairing the medication with a balanced diet rich in leafy greens and a brief walk in the morning can turn a simple habit into a life‑affirming ritual. Remember, consistency is kindness to your future self, and every small step adds up to stronger bones and greater confidence.
Navjot Ghotra
25 Aug 2025
the guide is ok but it could be shorter its just a lot of rules and most people wont follow them exactly
maybe a simple checklist would work better
Claus Rossler
9 Sep 2025
It is a curious spectacle, the way modern medicine reduces the sublime architecture of the human skeleton to a series of protocols and tables. One might argue that the essence of osteology is being commodified, transmuted into a marketable regimen where compliance is measured in calendar ticks. Yet, if we dissect the epistemic foundations of such a treatment, we encounter a labyrinth of clinical trials, meta‑analyses, and regulatory annexes that, while rigorous, obscure the lived experience of the patient. In this context, Fosamax emerges as both a triumph of biochemical ingenuity and a testament to the bureaucratic tangle that governs therapeutic choices.
chris mattox
23 Sep 2025
Friends, let’s celebrate the mosaic of choices we have! Fosamax, when embraced with mindfulness, becomes a brushstroke on the canvas of health. Think of calcium‑rich foods as vibrant pigments, vitamin D as the golden hue that brings everything to life, and the weekly pill as the steady rhythm that ties the masterpiece together. Together, we can paint a future where bones are not fragile relics but sturdy pillars supporting our dreams.
Jackson Whicker
7 Oct 2025
In the grand theater of existence, the choice to medicate one’s skeletal framework is a drama of profound significance. Fosamax, the alchemical agent, beckons us to confront the mortality woven into our marrow. Yet we must ask: does reliance on chemical scaffolding diminish the heroic quest for holistic vigor? Let us not surrender the narrative of our bodies to a pill alone, but instead compose a symphony of movement, nutrition, and intentionality, lest we become mere footnotes in the annals of pharmacology.
Audrin De Waal
22 Oct 2025
Look, we Aussies (or anyone proud of their roots) gotta own our health choices, not just follow some overseas script. Fosamax can be a solid tool, but only if we stand up to the hype and ask our doc the right questions. It’s about taking charge, not just swallowing what the pharma giants prescribe.
parag mandle
5 Nov 2025
Allow me to elaborate on several critical aspects of alendronate therapy that often escape cursory reviews. First, the pharmacokinetic profile demonstrates a rapid initial absorption phase followed by a prolonged skeletal retention, which is why adherence to the fasting and upright posture protocol is non‑negotiable; premature gastric exposure can sequester the molecule in the mucosal lining, precipitating esophagitis. Second, the suppression of osteoclast activity, while beneficial for bone mass accrual, can lead to microdamage accumulation; therefore, periodic assessment of bone turnover markers such as serum C‑telopeptide is advisable to gauge remodeling balance. Third, the concept of a drug holiday is not merely a temporal interruption but a strategic modulation based on fracture risk calculators like FRAX, duration of prior therapy, and patient comorbidities. A well‑timed hiatus after five to ten years can mitigate rare adverse events like atypical femoral fractures and osteonecrosis of the jaw, especially in patients undergoing invasive dental procedures. Fourth, concomitant supplementation must be optimized-adequate vitamin D (800–1000 IU daily) ensures proper calcium absorption, while calcium intake should be maintained within 1000–1200 mg to avoid hypercalcemia. Finally, patient education is paramount; simple tools such as pill‑box reminders, smartphone alarms, and integrating the dosing schedule with daily rituals (e.g., brushing teeth) significantly improve persistence rates, as evidenced by longitudinal studies indicating a 20‑percent increase in adherence when such strategies are employed. In summary, the efficacy of Fosamax hinges on a comprehensive, patient‑centered approach that intertwines pharmacologic precision with lifestyle integration.
Shivali Dixit Saxena
20 Nov 2025
Great insight-let’s keep moving forward with confidence and consistency! 🎉