Fake Generic Drugs: How Counterfeits Enter the Supply Chain

Every year, millions of people around the world take generic drugs because they’re affordable, effective, and widely available. But what if the pill you swallowed wasn’t made to help you - but to trick you? Fake generic drugs are not just a distant problem in developing countries. They’re slipping into supply chains everywhere, even in places with strong regulations. And they’re getting harder to spot.
How Fake Drugs Are Made
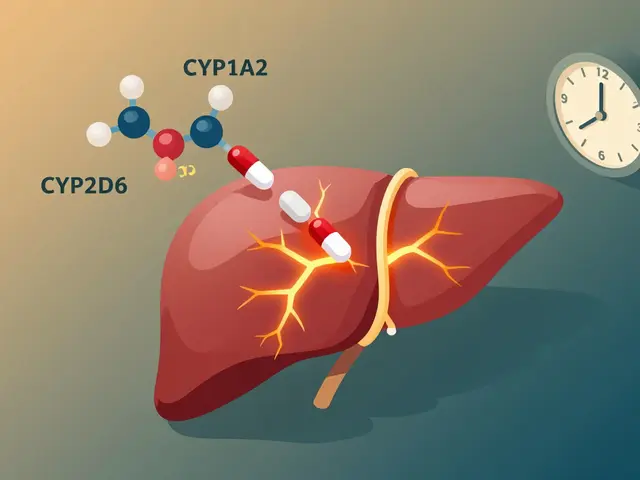
Counterfeit generic drugs don’t look like something out of a spy movie. They’re often perfect copies. The packaging looks identical. The tablets have the same color, shape, and imprint. But inside? The active ingredient might be missing, diluted, or replaced with something dangerous.
Most of these fake drugs come from unregulated factories, often hidden in warehouses across Southeast Asia, Eastern Europe, and parts of Africa. These aren’t underground labs with bubbling beakers. They’re small, legal-looking facilities that use off-the-shelf printing machines and chemical suppliers. Some even hire former employees of real drug manufacturers to replicate packaging down to the font size.
According to TrueMed Inc.’s 2023 analysis, 95% of counterfeit packaging is visually indistinguishable from the real thing. That means a pharmacist or patient might never notice - until it’s too late. One batch of fake antimalarial pills was found to contain only 10% of the needed artemisinin. The rest? Cornstarch and chalk. Patients didn’t get better. Some died.
How They Sneak Into Legitimate Supply Chains
Counterfeiters don’t need to break into hospitals or pharmacies. They exploit gaps in the system. There are three main ways fake drugs enter the legal supply chain:
- Parallel importation - A drug approved in Country A is bought legally, then resold in Country B where it’s not officially sold. Regulatory rules don’t match, so fake versions slip in as "alternatives."
- Grey market sales - Authorized distributors mix fake drugs with real ones. Why? Higher profits. A wholesaler might sell 90% real medication and 10% fake, and no one notices.
- Online pharmacies - The biggest loophole. The National Association of Boards of Pharmacy (NABP) found that 95% of online pharmacies operating without licenses sell fake drugs. These sites look professional. They have SSL certificates, customer reviews, and even fake "pharmacist" chatbots. People in the U.S., UK, and Canada order from them thinking they’re saving money - and end up with poison.
The 2008 heparin crisis showed how deep this problem runs. Heparin, a blood thinner, was contaminated with a cheap industrial chemical from a Chinese supplier. It made its way through multiple intermediaries, into U.S. hospitals, and caused 149 deaths. No one tested the raw material. No one questioned the supplier’s credentials. It was just another shipment.

Why Generic Drugs Are the Main Target
Branded drugs have patents, security features, and brand loyalty. Counterfeiters avoid them - too risky. But generics? They’re a goldmine.
Generic drug makers compete on price. That means thin margins. Many manufacturers cut corners. And when a batch fails quality checks, it gets discarded - or sold on the black market. Fake versions of these drugs are cheaper to produce because they skip testing, quality control, and regulatory filings.
The global generic drug market hit $438.7 billion in 2022. That’s a huge target. Counterfeiters focus on high-demand generics: antibiotics, blood pressure meds, diabetes drugs, and antimalarials. The U.S. Pharmacopeia’s database shows that over 28% of fake drug incidents involve cardiovascular medications. Why? Because people take them daily. If they don’t work, the patient doesn’t notice right away. By the time they do - it’s too late.
Why Detection Is So Hard
Here’s the scary part: most fake drugs aren’t caught because they’re not supposed to be.
Only 40% of countries have track-and-trace systems that can follow a drug from factory to pharmacy. Even fewer use serialization - unique codes on each package. As of January 2023, only 22 out of 194 WHO member states had fully working systems. That means a fake drug can travel across continents without leaving a digital trail.
And the fakes are getting smarter. Europol’s 2022 report found counterfeiters now use AI to generate perfect holograms, replicate batch numbers, and even mimic the texture of real blister packs. One operation in 2023 seized cancer drugs with AI-generated packaging that passed visual inspection by trained inspectors.
Pharmacists are overwhelmed. A 2022 survey by the International Pharmaceutical Federation found that 68% of pharmacists across 45 countries had seen suspected fake drugs. But 32% said they couldn’t tell the difference without lab testing. One pharmacist in Nigeria described receiving fake insulin with the same label, same color, same scent - but no active ingredient. She only found out after a patient went into a coma.

What’s Being Done - And What’s Not
Some progress is being made. The EU’s Falsified Medicines Directive, which took full effect in 2023, forced pharmacies to scan every package before dispensing. The result? A 18% drop in counterfeit drugs entering the legal supply chain in Europe.
Companies like Pfizer have spent nearly two decades building anti-counterfeiting programs. Since 2004, they’ve stopped over 302 million fake doses from reaching patients by working with customs, law enforcement, and distributors. But that’s just one company. Most generic manufacturers don’t have the budget for DNA tags, chemical tracers, or blockchain verification.
And here’s the catch: the tools that work - like digital verification systems - cost $0.02 to $0.05 per unit. For a $1 generic pill, that’s a 5% cost increase. Many manufacturers won’t pay it. So the cheapest drugs - the ones people rely on - are the most vulnerable.
What You Can Do
You can’t inspect every pill you take. But you can protect yourself:
- Buy from licensed pharmacies only. If you’re buying online, check the NABP’s Verified Internet Pharmacy Practice Sites (VIPPS) list. If it’s not on there, don’t trust it.
- Check the packaging. Compare it to your last prescription. Is the color off? Is the font slightly smaller? Are the numbers on the batch code different? These are red flags.
- Don’t ignore side effects. If a drug that always worked suddenly doesn’t - or makes you feel worse - talk to your doctor. It might not be your body changing. It might be the pill.
- Report suspicious drugs. In the U.S., use the FDA’s MedWatch system. In the UK, use the Yellow Card Scheme. Your report could stop a batch before it reaches others.
The truth is, counterfeit drugs won’t disappear until the system changes. Until every country requires serialization. Until every pharmacy scans every package. Until the cheapest drugs aren’t the most dangerous ones.
For now, awareness is your best defense. Because if you don’t know what you’re taking, you can’t know if it will save you - or kill you.



Comments (12)
Brad Ralph
11 Feb 2026
So basically, the system is designed to let people die quietly so someone can make an extra buck. Classic capitalism. 🤡
Suzette Smith
12 Feb 2026
I actually think this is way overblown. I’ve been on generics for years and never had an issue. Maybe you’re just paranoid?
Vamsi Krishna
13 Feb 2026
In India, we’ve seen this for decades. My uncle died because his BP meds were just sugar pills. They sold him a bottle labeled 'Amlodipine' but inside? Flour + turmeric. And guess what? The pharmacy owner laughed when he complained. 'You think they care about you?' he said. This isn’t a conspiracy - it’s a business model. And the West? They’re just now waking up because *they’re* being targeted now. The real tragedy? We’ve been screaming about this for 20 years. Nobody listened until it hit their pharmacy shelves.
steve sunio
14 Feb 2026
lmao so u mean to say that the usa has a drug supply chain? like... with regulations? lol. in nigeria we just buy from the guy who smiles and says 'it's original'. no labels, no receipts, just vibes. u guys are so extra.
Stephon Devereux
16 Feb 2026
This is why we need universal drug traceability. It’s not expensive - it’s cheaper than treating the side effects of fake meds. We’ve got the tech: blockchain, QR codes, AI verification. What we lack is the political will. If your blood pressure pill costs $1.50, but scanning it adds 3 cents - that’s not a cost. That’s an investment in human life. Stop treating healthcare like a commodity and start treating it like a right.
athmaja biju
16 Feb 2026
The real issue here is globalization. Why are we outsourcing our medicine production to countries that don’t even have clean water? This isn’t about fake drugs - it’s about surrendering our sovereignty. We used to make our own pills. Now we trust a factory in Bangladesh to decide if we live or die. And we wonder why people are angry.
Robert Petersen
18 Feb 2026
You’re not alone. I work in a pharmacy, and I’ve seen it too. Last month, a patient came in with a bottle of metformin that looked *almost* right - the font was off by 0.2mm. We called the manufacturer. Turns out it was fake. We reported it. And yeah, it felt good. Small wins. Keep speaking up. Someone’s life depends on it.
Carla McKinney
18 Feb 2026
I find it deeply disturbing that people still buy from online pharmacies. This isn’t a mystery. The FDA has a list. The NABP has a list. If you’re not using them, you’re choosing ignorance. And ignorance isn’t innocent - it’s complicity.
Sonja Stoces
18 Feb 2026
I knew it. I knew this was all a CIA plot. They let fake drugs in so people get sicker, then they sell the real ones at 10x the price. And the WHO? Totally in on it. They took money from Big Pharma to keep quiet. That’s why only 22 countries have trace systems - because the rest are controlled. Look up Operation Midnight Sun. They’ve been doing this since the 80s.
Annie Joyce
19 Feb 2026
I’m a pharmacist’s assistant. We get shipments daily. Most are fine. But once, a box of lisinopril had the wrong batch code - tiny detail, but it screamed 'fake'. We held it. Called the distributor. Turned out it was a mix-up from a distributor in Poland. They had no idea. We ended up destroying 400 bottles. No one thanked us. But we saved someone. Maybe. That’s enough.
Reggie McIntyre
21 Feb 2026
The real kicker? The counterfeiters are smarter than the regulators. They use AI to mimic packaging. They hire ex-employees. They exploit shipping loopholes. And we’re still using paper logs and handwritten invoices. We’re fighting the future with a typewriter. It’s not a crime problem - it’s a tech problem. We need real-time blockchain tracking on every blister pack. Not in 5 years. Now.
Autumn Frankart
22 Feb 2026
I’ve been taking my generic thyroid med for 8 years. I’m fine. So why are you scared? Maybe you’re just anxious. Or maybe you’ve been fed too much fear porn by the media. Not everything is a conspiracy. Sometimes a pill is just a pill.