Future Gallstone Treatment: Cutting-Edge Research & Technology

Gallstone Treatment Advisor
Personalized Gallstone Treatment Advisor
This tool helps identify the most appropriate gallstone treatment options based on your specific condition. Enter your information below to get personalized recommendations.
When Gallstone treatment looks beyond the operating theater, patients can expect fewer cuts, shorter stays, and smarter diagnostics. This article walks through the breakthroughs that could reshape how doctors dissolve, fragment, or even prevent gallstones over the next decade.
What doctors do today
Right now, the go‑to solution for symptomatic stones is cholecystectomy, usually laparoscopic. It removes the gallbladder and the stones it harbors, cutting down recurrence to almost zero. But the surgery still carries risks - bile leaks, infection, and a recovery window of 1‑2 weeks.
For patients who can’t tolerate surgery, doctors sometimes prescribe ursodeoxycholic acid (UDCA). This bile‑acid pill slowly dissolves cholesterol stones, but the process can take months to years and works only on gallstone types that are small and radiolucent.
Endoscopic methods, such as endoscopic retrograde cholangiopancreatography (ERCP), can retrieve stones from the common bile duct, yet they are technically demanding and carry a 3‑5% pancreatitis risk.
gallstone treatment is therefore a mix of surgery, medication, and endoscopy - effective but not always ideal.
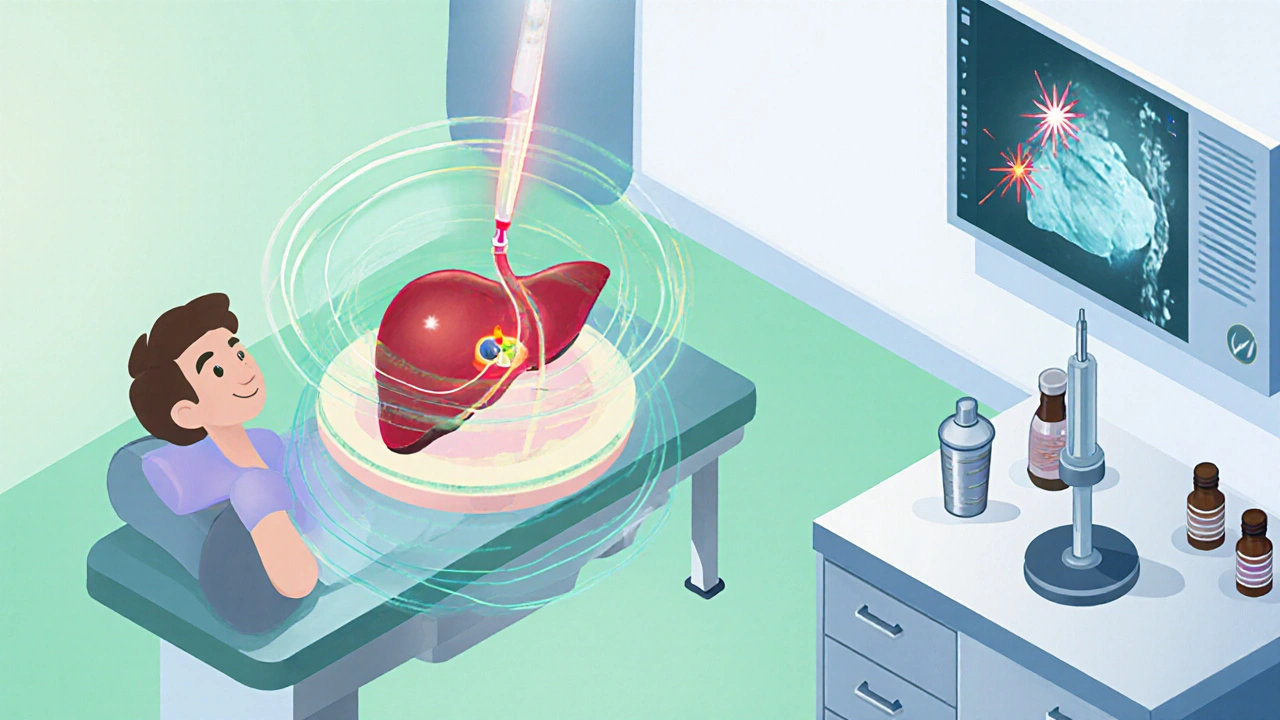
Non‑invasive lithotripsy gains traction
Traditional lithotripsy uses shock waves to crush kidney stones. Recent trials adapt the technology for gallstones, delivering focused ultrasound through the liver tissue. Early 2025 data from a multicenter European study showed a 78% stone‑free rate after two sessions, with virtually no pain.
Even more precise is laser lithotripsy. Mini‑fibers inserted via a tiny percutaneous tract emit pulsed laser energy that vaporizes stone material. The method reduces the need for any incision and allows real‑time imaging feedback.
- Advantages: outpatient setting, no general anaesthesia, < 30‑minute procedure.
- Current limitations: equipment cost, required expertise, suitability mostly for solitary stones < 2 cm.
Next‑generation bile‑acid therapies
Researchers are engineering synthetic bile acids that outperform UDCA. A 2024 Phase‑II trial of obeticholic acid (OCA) combined with a novel transporter inhibitor cut stone volume by 45% in six months, even for mixed cholesterol‑pigment stones.
Beyond drugs, scientists are exploring probiotic cocktails that modify gut microbiota to lower cholesterol saturation in bile. A Taiwanese cohort who took a 12‑week synbiotic blend showed a 30% reduction in new stone formation.
Artificial intelligence reshapes diagnosis
High‑resolution MRI and CT generate massive image datasets. Artificial intelligence models trained on 200,000 scans can now differentiate cholesterol from pigment stones with 94% accuracy, flagging asymptomatic patients who might benefit from early therapy.
AI also predicts which patients will fail UDCA therapy, allowing doctors to shortcut to lithotripsy or surgery before complications arise.
Nanoparticle drug delivery - targeting the stone
Nanocarriers coated with gallbladder‑specific ligands ferry bile‑acid analogues directly to the stone surface. In a 2025 animal model, a single IV dose of lipid‑based nanoparticles reduced stone size by 60% within two weeks, with negligible systemic side effects.
This approach could merge the convenience of pills with the potency of localized therapy, a game‑changer for patients with multiple tiny stones.
Regenerative and bioengineered solutions
For the rare cases where the gallbladder must be removed, researchers are investigating tissue‑engineered gallbladders. Using a patient’s own stem cells seeded onto a biodegradable scaffold, a 2023 pilot showed functional bile storage in 3 out of 5 subjects after one year.
While still experimental, this avenue hints at a future where removal isn’t the final answer - the organ could be rebuilt, eliminating long‑term digestive changes.

How the new options stack up
| Aspect | Traditional Surgery | Shock‑wave Lithotripsy | Laser Lithotripsy | Advanced Bile‑Acid Therapy | Nanoparticle Delivery |
|---|---|---|---|---|---|
| Invasiveness | High (incision) | Low (outpatient) | Very Low (percutaneous) | Low (oral) | Very Low (IV) |
| Recovery time | 7‑14 days | Same day | 1‑2 days | Weeks to months | Hours |
| Stone‑free rate | ~99% | 78% (multiple sessions) | 85% (single session) | 30‑45% reduction | 60% reduction (early trials) |
| Typical candidates | All symptomatic | Solitary < 2 cm | Solitary < 2 cm, high‑risk surgery | Cholesterol stones, early disease | Multiple small stones, contraindicated surgery |
What patients can expect in the next five years
By 2030, most hospitals will have a dedicated gallstone‑center offering a menu of options. The typical pathway could look like this:
- AI‑driven imaging classifies stone type and predicts treatment response.
- If suitable, an outpatient shock‑wave session is scheduled.
- For resistant stones, a laser fiber is inserted percutaneously under local anaesthesia.
- Patients who can’t undergo any energy‑based method receive a targeted nanoparticle infusion.
- Only those who still have large or complicated stones proceed to minimally invasive cholecystectomy.
The result is a personalized, step‑wise plan that minimizes pain, cuts costs, and reduces the number of people needing full surgery.
Key takeaways
- Non‑invasive lithotripsy and laser techniques are moving from niche to mainstream.
- New bile‑acid drugs and probiotic regimens can shrink stones without cuts.
- AI boosts diagnostic accuracy and helps choose the right therapy early.
- Nanoparticle carriers promise rapid stone reduction with minimal side effects.
- Regenerative gallbladder research could eventually replace removal altogether.
Can shock‑wave lithotripsy replace surgery for all gallstones?
Not yet. It works best for solitary cholesterol stones under 2 cm and requires a clear acoustic window. Larger or calcified stones still need surgical removal.
Is ursodeoxycholic acid still useful?
Yes, but its role is shrinking. New agents like obeticholic acid are more potent, yet UDCA remains the first‑line oral option for small, radiolucent stones.
How safe are nanomedicine approaches?
Early animal studies show low systemic toxicity because the particles target bile‑acid transporters. Human trials are slated for 2026, so safety data are still emerging.
Will AI replace the radiologist?
AI acts as a decision‑support tool, flagging suspicious stones and predicting treatment response. Radiologists still interpret images and integrate clinical context.
What’s the outlook for patients who can’t have surgery?
For high‑risk patients, outpatient lithotripsy, laser fiber therapy, or targeted nanoparticle infusions provide viable alternatives, dramatically lowering the need for invasive procedures.






Comments (11)
jagdish soni
19 Oct 2025
One can contemplate the arc of medical progress as a reflection of our collective yearning to master nature and transcend the constraints of flesh and stone. The emergence of lithotripsy for gallstones echoes the ancient alchemical dream of turning the impossible into the mundane. In the quiet of a modern outpatient suite the shock waves ripple through hepatic tissue like a poet’s syllable across a silent page. Yet beneath this veneer of technology lies a discipline that still respects the stubbornness of calcium bonded to cholesterol. The promise of non‑invasive interventions is not merely a convenience but a statement of humility before the body’s own chemistry. When AI discerns the composition of a stone it is performing a kind of digital divination, a seer interpreting the hidden signatures of disease. The synthetic bile‑acid agents, crafted in laboratories, are the modern equivalent of the philosopher’s stone, seeking to dissolve the hardened remnants of our diets. Nanoparticle carriers glide through the bloodstream like microscopic couriers, delivering their payload with surgical precision. Each of these advances invites us to question whether removal of the gallbladder is truly the final act or merely a prelude to regeneration. Regenerative scaffolds seeded with stem cells whisper of a future where organs can be reborn from the patient’s own cells, a concept that would have seemed heretical a generation ago. As practitioners, we must balance the allure of cutting‑edge tools with the wisdom of time‑tested surgery, remembering that a 99% stone‑free rate still carries the weight of certainty. The interdisciplinary tapestry woven by surgeons, engineers, microbiologists, and data scientists is a tribute to the collaborative spirit of modern medicine. While the early data on laser lithotripsy shows an 85% stone‑free rate, we must remain vigilant about the learning curve and resource allocation. It is tempting to view these technologies as panaceas, yet each carries its own set of indications, limitations, and cost considerations. The patient’s voice, often drowned in clinical jargon, must be amplified as we chart the path forward. In the end, the true measure of progress will be how these innovations reshape quality of life, reduce postoperative pain, and democratize access to care across socioeconomic divides. The future of gallstone treatment, therefore, is not a single breakthrough but a symphony of advances, each contributing its unique timbre to the melody of healing.
parth gajjar
21 Oct 2025
The drama of a solitary stone shattering under focused ultrasound feels almost mythic in its simplicity. It is a striking reminder that not every battle requires a scalpel, only the right pulse of energy. The data showing a 78% stone‑free rate after two shock‑wave sessions hints at a paradigm shift for patients who dread an operating room. Still the method demands a clear acoustic window, a nuance that can be lost in headlines. As we embrace these tools we must also respect the skill required to align them precisely.
Maridel Frey
23 Oct 2025
For clinicians seeking to integrate these emerging therapies, it is essential to develop multidisciplinary protocols that include radiology, gastroenterology, and surgery. Training programs should incorporate hands‑on workshops for shock‑wave and laser lithotripsy to ensure competency. Additionally, patient education materials must be updated to reflect the benefits and limitations of each option.
Madhav Dasari
25 Oct 2025
Seeing the range of new options is genuinely uplifting, especially for those fearful of surgery. The idea that a simple outpatient session could dissolve a stone brings hope to many. Even the probiotic approaches feel like nature lending a hand to our bodies. Of course, each treatment has its sweet spot, and we must match patients carefully. I’m excited to see how these advances will lower the overall burden of gallstone disease.
DHARMENDER BHATHAVAR
26 Oct 2025
This concise update highlights key points: non‑invasive lithotripsy, laser fiber, AI diagnostics, nanoparticle delivery. Each offers reduced recovery time and targeted therapy. Adoption will depend on cost and training.
ashanti barrett
28 Oct 2025
It is noteworthy that AI models now achieve 94% accuracy in stone type classification, an improvement that can streamline treatment pathways. Targeted nanoparticle delivery also shows a 60% reduction in stone size within weeks, potentially sparing patients from invasive procedures. These advances underscore the importance of continued investment in translational research. The community should monitor upcoming human trials closely.
Leo Chan
30 Oct 2025
Hopeful vibes for all those avoiding the scalpel.
Latasha Becker
31 Oct 2025
From a pharmacokinetic standpoint, the lipid‑based nanocarriers exploit bile‑acid transporters to achieve preferential deposition on calculi, thereby maximizing local drug concentration while minimizing systemic exposure. Moreover, the synthetic analogs of obeticholic acid exhibit higher affinity for the farnesoid X receptor, translating into a more robust downregulation of hepatic cholesterol synthesis pathways. The integration of such molecular mechanisms with advanced imaging algorithms enhances predictive modeling of therapeutic response. Nonetheless, the economic implications of scaling nanoparticle production warrant a thorough cost‑benefit analysis. Future discourse should address regulatory pathways for nanomedicine approvals.
Kevin Sheehan
2 Nov 2025
The philosophical underpinning of AI‑augmented diagnosis raises questions about the balance between algorithmic precision and clinical intuition. While the models boast high accuracy, they remain tools, not replacements for seasoned judgment. It is crucial to maintain a collaborative dynamic where the physician interprets AI outputs within the broader context of patient history. This synergy can ultimately enhance outcomes without eroding the art of medicine.
Jay Kay
4 Nov 2025
Honestly, the hype around laser lithotripsy seems overblown. The stone‑free rate is decent but not revolutionary compared to traditional surgery. Most patients will still end up in the OR.
Jameson The Owl
6 Nov 2025
Consider for a moment the broader geopolitical context in which these medical technologies emerge, a landscape where pharmaceutical conglomerates and state‑funded research institutions engage in a subtle dance of influence and control that often escapes the public eye; the advancement of nanomedicine, for instance, is not merely a scientific triumph but also a manifestation of strategic investment aimed at consolidating economic power within a select cadre of global elites, and as such the claims of safety and accessibility must be scrutinized through a lens that accounts for potential conflicts of interest and the ever‑present risk of technological dependency on proprietary platforms, which could, in the long run, erode the autonomy of independent practitioners and patients alike, especially when regulatory frameworks lag behind the rapid pace of innovation, leaving gaps that can be exploited for profit-driven agendas; therefore, while the reported 60% reduction in stone size via targeted nanoparticle infusion is indeed impressive, it is incumbent upon the medical community to demand transparency, rigorous independent trials, and equitable distribution mechanisms, lest we find ourselves complicit in a system that privileges cutting‑edge treatments for a privileged few while marginalizing those without the means to access such advancements.