How to Coordinate Multiple Prescriptions to Avoid Conflicts

More than one in three adults over 60 are taking five or more prescription drugs at once. That’s not just common-it’s risky. Every pill you take has the potential to clash with another, turning a treatment into a danger. Dry mouth, dizziness, stomach bleeding, kidney stress-these aren’t just side effects. They’re warning signs of something worse: a drug interaction that could land you in the hospital. And it’s not just about what your doctor prescribed. Those vitamins, herbal teas, or over-the-counter painkillers? They’re part of the mix too. The good news? You don’t have to manage this alone. With the right system, you can cut the risk, save money, and feel more in control.
Start with a complete, updated medication list
You can’t fix what you don’t see. Most people think they remember all their meds-until they sit down and try to write them all out. That’s when they realize they forgot the ibuprofen they take for knee pain, the magnesium supplement, or the sleep aid their cousin swore by. A full list isn’t optional. It’s your first line of defense.Every item needs four things: the exact name (brand and generic), the dose, when to take it, and why. For example: Lisinopril 10mg, once daily in the morning, for high blood pressure. Don’t write ‘blood pressure pill.’ Be specific. Include everything-even the stuff you only take once in a while. If you’ve taken it in the last 30 days, it belongs on the list.
Update this list every time you get a new prescription, stop one, or change the dose. Keep a printed copy in your wallet and a digital version on your phone. Share this list with every doctor, pharmacist, and caregiver. If you’re seeing multiple specialists, this is the only thing that keeps them all on the same page.
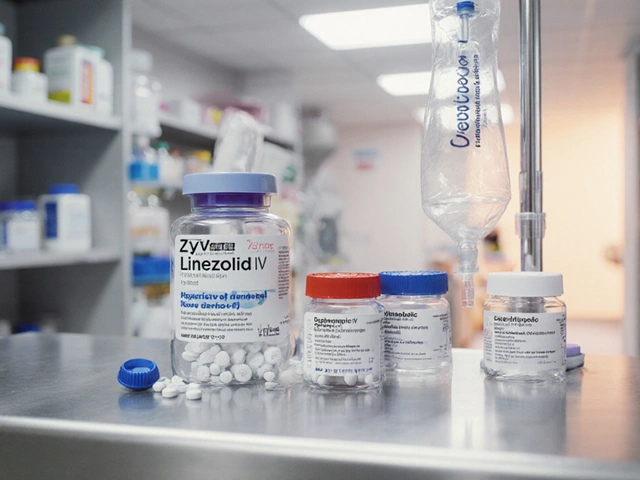
Use one pharmacy for everything
Switching pharmacies because one is closer or cheaper sounds smart-until a drug interaction slips through the cracks. Pharmacists are trained to spot dangerous combinations. But they can only do that if they see your full history.A 2023 study in Health Affairs found that single-pharmacy users had a 47% higher chance of catching a risky interaction than people who split prescriptions between two or more pharmacies. Why? Because each pharmacy only sees part of your story. One might know you’re on blood thinners. The other doesn’t know you’re also taking St. John’s Wort-which can make your blood thinner dangerously strong.
Stick with one pharmacy. Even if it’s a 15-minute drive. Let them build your complete profile. Ask them to run a full medication review at least once a year. Many pharmacies now offer this for free, especially if you’re on Medicare Part D. They’ll check for duplicates, interactions, and whether any pills are no longer needed.
Sign up for medication synchronization
Imagine getting all your monthly prescriptions ready on the same day-no more juggling refill dates, missed doses, or running out of one med while another’s still full. That’s medication synchronization. It’s not a fancy app. It’s a simple, proven system offered by most community pharmacies.Here’s how it works: You pick one day each month-say, the first Thursday. The pharmacy adjusts your refill schedules so everything’s ready on that day. If your blood pressure pill is due on the 5th and your cholesterol med on the 12th, they’ll give you an extra week’s supply of the first one so they line up. You pick up everything at once. No more calls, no more confusion.
Studies show this cuts missed doses by 31% and reduces hospital visits by 22%. It’s especially helpful if you’re on three or more maintenance meds. Ask your pharmacist if they offer it. Most do. If they don’t, ask them to start. It’s a low-cost, high-impact change.

Use a pill organizer-smartly
A pill organizer isn’t just for seniors. It’s for anyone juggling multiple pills. But not all organizers are equal. A basic 7-day box with AM/PM slots is a huge step up from trying to remember what you took at 8 a.m. versus 8 p.m.Look for one with clear labels and separate compartments. Fill it once a week-Sunday evening works well for most people. Do it while watching TV. Make it part of a routine. Studies show people who fill their organizer during a consistent daily ritual improve adherence by 33%.
For extra help, consider an alarm-enabled organizer like Hero Health or MedMinder. These devices beep, flash, and even call a family member if you miss a dose. They cost $500-$900, but many Medicare Advantage plans cover them if you have a history of non-adherence. If cost is an issue, ask your pharmacist about loaner programs or community grants.
Know the red flags and when to act
Some side effects are normal. Others are red flags. If you start feeling unusually tired, confused, dizzy, or have stomach pain after starting a new med or changing a dose-don’t wait. Call your pharmacist or doctor right away.Common dangerous combinations include:
- NSAIDs (like ibuprofen) with blood pressure meds-can cause kidney damage
- Calcium supplements with thyroid medication-calcium blocks absorption if taken together
- St. John’s Wort with antidepressants-can cause serotonin syndrome, a life-threatening condition
- Antibiotics with birth control pills-can reduce effectiveness
Also, never assume a supplement is safe just because it’s natural. The American Geriatrics Society warns that 82% of dangerous interactions happen because patients don’t tell their doctors about vitamins or herbs. Write them down. Show them. Don’t leave them out.
Ask about deprescribing
Just because you were prescribed something years ago doesn’t mean you still need it. Medications can become unnecessary as your health changes. A pill that helped with pain after surgery might not be needed now. A cholesterol drug might be safe to lower if your levels improved.Ask your doctor: “Is this still necessary?” or “Could any of these be stopped?” This is called deprescribing-and it’s a critical part of safe polypharmacy management. The American Geriatrics Society’s 2023 Beers Criteria lists 30 high-risk medications and combinations that should be avoided in older adults. Many of them are still being prescribed because no one ever checked.
Don’t stop anything on your own. But do ask. Your pharmacist can help you prepare questions for your doctor. They’ll know which meds are most likely to be safely reduced or eliminated.
Use digital tools-but don’t rely on them alone
Apps like Medisafe, MyMeds, or CVS’s pharmacy app can send reminders, track refills, and even alert you to interactions. In a 2022 JAMA study, users of these apps had 28% better adherence than those using paper logs.But here’s the catch: 62% of adults over 75 don’t use smartphones regularly. If you or a loved one struggles with tech, don’t force it. A printed list and a pill organizer are more reliable than an app you never open.
Use digital tools only if they fit your life. If you’re comfortable with your phone, set reminders for every dose. If not, stick with the old-school methods. They work.
Know your rights and resources
If you’re on Medicare Part D and take eight or more medications for two or more chronic conditions, you’re eligible for free Medication Therapy Management (MTM). This is a 20-30 minute session with a pharmacist who reviews every pill you take, checks for problems, and gives you a written plan.In January 2024, CMS started paying pharmacists $150 per MTM session for high-risk patients. That means pharmacies have every reason to reach out to you. If you haven’t been contacted, call your pharmacy and ask. You’re entitled to this service.
Also, ask about patient assistance programs. Some drug manufacturers offer free or low-cost meds if you qualify. Your pharmacist can help you apply.
Make this a habit, not a chore
Coordinating prescriptions isn’t a one-time task. It’s a lifelong practice. Treat it like brushing your teeth. Do it regularly. Update your list after every doctor visit. Check your organizer every Sunday. Ask questions at every refill. Don’t wait for a problem to happen.The cost of not doing this is staggering. In the U.S., medication errors cause 277,000 deaths a year and cost $300 billion in avoidable care. But the fix is simple: stay organized, stay informed, and stay in control.
You don’t need to be a medical expert. You just need to be consistent. And you’re not alone. Pharmacists, nurses, and care teams are ready to help. All you have to do is ask.


Comments (10)
Eileen Reilly
11 Jan 2026
omg i just realized i’ve been taking melatonin AND benadryl for sleep and didnt even think to check if they clash… my pharmacist is gonna kill me. thanks for the wake up call. updated my list right now.
Monica Puglia
13 Jan 2026
so glad someone finally said this 🙌 i’ve been telling my mom for years to use one pharmacy but she keeps switching because ‘this one has better deals’… now i’m sending her this post. also, the pill organizer with alarms? life changer. got one for my grandma and she hasn’t missed a dose in 4 months. 💙
Cecelia Alta
13 Jan 2026
ugh i’m so tired of these ‘simple solutions’ articles. yeah sure, ‘use one pharmacy’ - what if you live in a town with one crappy pharmacy that can’t even spell ‘lisinopril’? and ‘medication sync’? good luck getting that to work when your doc changes your dose every two weeks. this whole thing is just band-aid advice for people who won’t do the real work: fire their doctors and get a geriatric pharmacist on retainer. also, st john’s wort? everyone knows that’s a death cocktail with SSRIs. why is this even news?
steve ker
14 Jan 2026
This is why americans die early. Too many pills. Too many doctors. Too many apps. Just take less. Simple. No magic. No lists. Just stop.
George Bridges
15 Jan 2026
I’ve worked with elderly patients for 18 years and this is the most practical guide I’ve seen. The deprescribing point is critical - so many are on meds they don’t need anymore, and no one ever asks. Also, the MTM benefit under Medicare? Most people don’t know it’s free. I always tell my clients to call their pharmacy and say ‘I want my Medication Therapy Management session.’ They’ll schedule it right away.
Rebekah Cobbson
17 Jan 2026
For anyone feeling overwhelmed - you don’t have to do it all at once. Start with one thing. Write down your meds tonight. Just one list. That’s your win. Then next week, call your pharmacy and ask about sync. Then maybe get a pill organizer. Baby steps. You’ve got this. And if you need help? Text me. I’ll sit with you and make the list. No judgment. Just support.
Audu ikhlas
19 Jan 2026
Nigeria we have one pharmacy and one doctor and we dont need 10 pills to live. You americans are so weak. Your body cant handle one aspirin without 3 other pills to fix the side effects. This is why your life expectancy is falling. Stop taking so much crap.
Sonal Guha
20 Jan 2026
The real issue is doctors prescribing without checking interactions. Pharmacists are the last line of defense but they're not paid enough to do proper reviews. This post puts the burden on patients when it should be on the system. Also why is st john's wort even sold over the counter? It should be banned.
TiM Vince
21 Jan 2026
I’m 78 and don’t use apps. I have a binder. Every med, every supplement, every OTC - written by hand. I update it after every visit. I keep it in my coat pocket. I hand it to every new doctor. Simple. No Wi-Fi needed. Works every time. The tech stuff? Nice for some. But if you can’t use it, don’t stress. Paper still wins.
Jessica Bnouzalim
22 Jan 2026
YESSSSS to the pill organizer with alarms!!! I got one for my dad after he almost went to the ER because he took his blood thinner twice… and now he calls it his ‘robot nurse’ 😭 also - deprescribing? I asked my grandma’s doctor if she still needed that anxiety med from 2012… he said ‘oh wow, we forgot to take her off that.’ she’s been so much calmer since stopping it. ask the question - you might save their life.