How to Handle Missed Pediatric Medication Doses Safely

Missing a dose of your child’s medication happens. It’s not a failure. It’s not even rare. But how you respond can make a big difference - or cause real harm. The biggest mistake? Doubling up. That’s not just risky; it’s dangerous. Kids aren’t small adults. Their bodies process medicine differently. A dose that’s safe for an adult could overdose a 5-year-old. And if you’re unsure what to do, you’re not alone. Most parents don’t know the rules. A 2022 survey from the Children’s Hospital of Philadelphia found that 41% of parents couldn’t tell when to give a missed dose and when to skip it - even for twice-daily meds. For three-times-daily meds? That number jumped to 68%.
Don’t Double the Dose - Ever
Let’s get this out of the way first: never double a pediatric dose. Not for antibiotics. Not for asthma inhalers. Not even for Tylenol. The idea of ‘making up’ for a missed dose feels logical. But it’s deadly wrong. Children’s kidneys and livers are still developing. They can’t clear drugs the way adults can. Dr. Sarah Verbiest’s 2023 review found that doubling doses increases the risk of severe reactions in kids under 12 by 278%. That’s not a small risk. That’s an emergency waiting to happen.
Think about it this way: if your child missed a 5 mL dose of amoxicillin at 8 a.m., and it’s now 10 a.m., giving 10 mL at 10 a.m. doesn’t fix the problem - it creates a new one. You’re flooding their system with a drug they weren’t supposed to get all at once. The result? Vomiting, drowsiness, low blood pressure - or worse. Hospitals see this. The American Academy of Pediatrics says medication errors cause 11% of preventable harm in pediatric hospitals. Over half of those are dosing mistakes. And doubling is the top culprit.
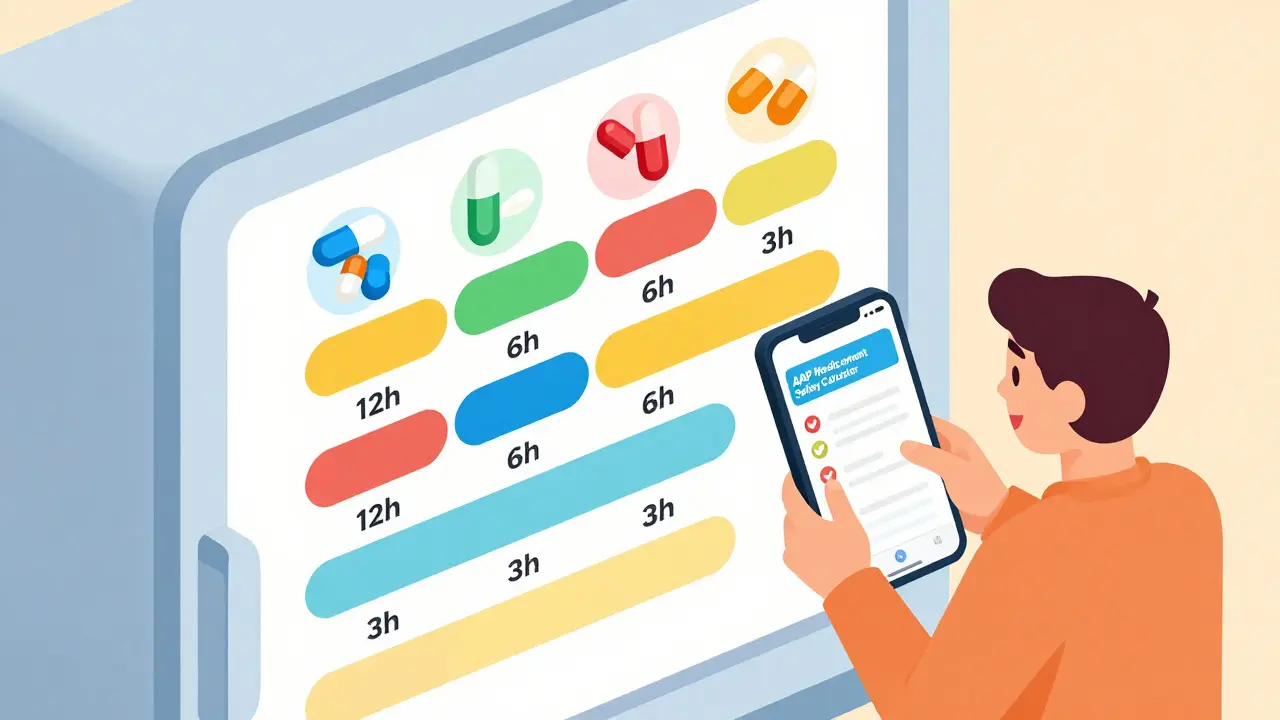
Time-Based Rules: What to Do Based on Dosing Schedule
The real answer isn’t guesswork. It’s timing. Most hospitals use clear, science-backed thresholds based on how often the medicine is given. These aren’t arbitrary. They’re built from how long drugs stay active in a child’s body.
- Once-daily meds (like some antibiotics or seizure drugs): If you remember within 12 hours of the missed time, give it. If it’s been more than 12 hours, skip it. Don’t give it the next morning. Just go back to your regular schedule. Giving it late can throw off the whole cycle.
- Twice-daily meds (like some asthma or ADHD meds): If you remember within 6 hours of the missed dose, give it. If it’s been more than 6 hours, skip it. For example, if the dose is due at 8 a.m. and 8 p.m., and you remember at 3 p.m., give it. But if it’s 10 p.m. and you forgot the morning dose, skip it. The next dose is coming in 2 hours.
- Three-times-daily meds (like some antibiotics or pain meds): Use a 3-hour window. If you remember within 3 hours of the missed time, give it. If it’s been longer, skip it. Don’t try to squeeze in a third dose if you’re already late for the next one.
- Four-times-daily or every 6 hours: If you miss a dose by more than 2 hours, skip it. These are often critical meds - like insulin or seizure drugs. Giving them too close together can cause dangerous drops in blood sugar or breathing problems.
- Every 2-4 hours (like pain meds after surgery): If it’s been more than 2 hours since the last dose, skip the missed one. Don’t wait for the next scheduled time. Just give the next one on schedule. This is common in hospitals and emergency settings. Overdosing here can lead to respiratory depression - especially with opioids like morphine.
These aren’t just suggestions. They’re from Children’s Wisconsin, Cincinnati Children’s, and other top pediatric hospitals. They’re based on pharmacokinetics - how the body absorbs, uses, and clears the drug. The goal isn’t perfection. It’s safety.
Special Cases: Oncology, High-Risk, and Complex Meds
Some meds are different. If your child is on chemotherapy, immunosuppressants, or other high-risk drugs, the rules change. For cancer treatment, even one missed dose can reduce effectiveness. In these cases, call the oncology team immediately. Don’t wait. Don’t guess. Don’t rely on general guidelines. Their protocol is specific to your child’s treatment plan.
Also, watch for ‘red’ category meds. These are high-risk drugs - like insulin, heparin, or certain seizure medications - where the FDA found that 25% of product leaflets don’t even include missed dose instructions. That’s a gap. If your child’s medication is on this list, ask your pharmacist or doctor for written guidance. Don’t assume the label says enough.
Children with complex medical needs - those on four or more daily medications - are at 300% higher risk for errors, according to the Canadian Pediatric Society. For them, simple mistakes multiply. That’s why color-coded charts, digital reminders, and caregiver training matter so much. Boston Children’s Hospital reduced missed doses by 44% just by switching to color-coded dosing schedules. If your child has multiple meds, ask your care team if they offer these tools.
How to Avoid Missed Doses in the First Place
Prevention beats correction. Here’s what works:
- Use an oral syringe, not a spoon. The FDA says teaspoon and tablespoon confusion causes 22% of dosing errors. A syringe gives you exact measurements. Even if the bottle says ‘use the cap,’ ditch it. Caps are inaccurate.
- Set phone alarms for each dose. Label them clearly: ‘Amoxicillin - 8 a.m.’ Not just ‘Medicine.’
- Keep a written log. Note the time you gave each dose. If you miss one, you’ll know exactly when it happened.
- Use the Pediatric Medication Safety Calculator app from the American Academy of Pediatrics. It’s free. You enter the drug, frequency, and time missed - and it tells you what to do. Beta testers saw an 83% improvement in decision accuracy.
- Teach-back method: After your doctor explains the schedule, ask your child’s caregiver - or even your child if they’re old enough - to repeat it back. If they can’t explain it clearly, ask again. Cincinnati Children’s cut missed dose errors by 37% using this method.
What to Do When You’re Still Unsure
You’re not expected to know everything. Even nurses get confused sometimes. If you’re stuck, here’s what to do:
- Check the medication label. Look for ‘What if I miss a dose?’ section. If it’s missing, call the pharmacy.
- Call your child’s doctor or pharmacist. Don’t wait until morning. Most offices have an after-hours line.
- Use the AAP app. It’s designed for this exact scenario.
- If your child shows signs of overdose - drowsiness, trouble breathing, vomiting, seizures - call 999 or go to A&E immediately. Don’t wait.
Remember: it’s always safer to skip a dose than to give too much. Your instinct to ‘make it up’ is understandable. But in pediatrics, that instinct can kill. The system isn’t perfect. Labels are unclear. Instructions are vague. But you can protect your child by knowing the rules and trusting them - even when it feels wrong.
Real Talk: What Parents Actually Do
Reddit and parenting forums are full of stories. One parent wrote: ‘I doubled the antibiotic because I didn’t want the infection to come back.’ Another said: ‘I gave the seizure med 2 hours late, then gave the next one early because I was scared.’ These aren’t bad parents. They’re tired, anxious, overwhelmed. And they’re following gut feelings, not science.
But here’s the truth: giving a little less, on time, is better than giving too much, all at once. Medications work best when they’re steady. A 10% gap in dosing is far less dangerous than a 100% overdose. The body can handle a little delay. It can’t handle a spike.
Parents of children with complex conditions report 2.7 times more medication errors than those with healthy kids. That’s not because they’re careless. It’s because the system is complicated. You’re juggling multiple meds, multiple times a day, often with unclear instructions. That’s not your fault. But you can take control - by learning the rules, using tools, and asking for help.
What’s Changing for the Better
There’s progress. The FDA is now requiring all pediatric medications to include clear missed dose instructions. The Institute for Safe Medication Practices is adding pictograms to labels - simple icons showing ‘skip if more than 3 hours late.’ Smart dispensers are rolling out, cutting missed doses by 68% in trials. AI tools like the NIH’s PediMedAI project are testing alerts that warn caregivers 30 minutes before a dose is due. In rural areas, where access to specialists is limited, these tools could be lifesavers.
But the biggest change? It’s not tech. It’s awareness. More hospitals are training parents using teach-back methods. More pharmacists are asking: ‘Do you know what to do if you miss a dose?’ That simple question is saving lives.
What should I do if I miss my child’s antibiotic dose?
If it’s been less than 12 hours since the missed dose (for once-daily), give it. If it’s been more than 12 hours, skip it and continue with the next scheduled dose. Never double the dose. For twice-daily antibiotics, use a 6-hour window. Always check the label or call your pharmacist if unsure.
Can I give a missed dose if it’s almost time for the next one?
No. If it’s within 2-6 hours of the next dose (depending on frequency), skip the missed one. Giving two doses too close together can lead to overdose. The goal is to keep levels steady, not to catch up. Your child’s body needs time between doses to process the medicine safely.
Is it safe to use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary in size and are inaccurate. The FDA warns that teaspoon and tablespoon confusion causes 22% of pediatric dosing errors. Always use the oral syringe or measuring cup that came with the medicine. If you lost it, ask your pharmacy for a new one - they’re usually free.
What if my child vomits right after taking the medicine?
If your child vomits within 15-20 minutes of taking the dose, it’s likely the medicine didn’t get absorbed. Call your doctor or pharmacist. They may advise giving another full dose. If vomiting happens after 20-30 minutes, the medicine was probably absorbed - don’t give more. Never guess. Always check with a professional.
Are there apps that help track pediatric doses?
Yes. The American Academy of Pediatrics launched a free Pediatric Medication Safety Calculator app. It tells you what to do when a dose is missed based on the drug, frequency, and time. Beta testers improved decision accuracy by 83%. Other apps like Medisafe and MyTherapy also offer pediatric features, including reminders and dose logs.
How do I know if a medication is high-risk?
High-risk (‘red’ category) meds include insulin, chemotherapy, opioids, seizure drugs, and anticoagulants. These are drugs where even small errors can cause serious harm. If your child is on one of these, ask your doctor or pharmacist for written instructions on missed doses. Also, look for pictograms on the label - newer versions now include icons showing time thresholds.
What should I do if I’m still unsure after checking everything?
Call your child’s doctor, pharmacist, or NHS 111. Don’t wait. Most pharmacies have a 24/7 line. When in doubt, skip the dose. It’s safer than giving too much. Write down what happened and bring it up at your next appointment. You’re not alone - this happens to families every day.





Comments (12)
Swapneel Mehta
19 Dec 2025
Been there. Missed my daughter's antibiotic dose twice last month. Didn't double it. Just waited. She didn't die. The system works if you don't panic.
Christina Weber
20 Dec 2025
There's a glaring omission here: the FDA doesn't require missed-dose instructions on pediatric meds. Not yet. That claim is misleading. The proposed rule is still in public comment. Please stop spreading misinformation, even if it's well-intentioned.
Dan Adkins
20 Dec 2025
It is imperative to underscore, with the utmost gravity, that the administration of pediatric pharmaceuticals must adhere to strictly calibrated pharmacokinetic parameters as established by peer-reviewed clinical protocols. The notion of improvisation in dosing regimens constitutes a grave deviation from evidence-based medical practice and is, in essence, a form of negligent endangerment.
Grace Rehman
22 Dec 2025
So we're supposed to trust a chart that says 'skip if over 3 hours' but not trust our own instincts when our kid's fever spikes? Funny how science always wins... until it doesn't. 🤷♀️
Jay lawch
22 Dec 2025
Let me guess - this whole thing was written by someone who’s never had to juggle four meds while working two jobs and raising a kid with autism. They talk about ‘color-coded charts’ like it’s a magic fix. Meanwhile, in rural India, parents use kitchen spoons because pharmacies are 80 miles away and the only label says ‘give once daily’ with no time. This isn’t about safety - it’s about privilege. The system isn’t broken. It was designed this way to keep the poor guessing.
Cara C
22 Dec 2025
I love how this post doesn’t shame parents. That’s rare. I missed my son’s seizure med once because I was changing a diaper and the clock got confusing. I called the pharmacy. They said skip it. I cried. Then I made a reminder sticker with a picture of a clock. Now we’re good. You’re not failing. You’re learning.
Teya Derksen Friesen
22 Dec 2025
As a pediatric nurse in Toronto, I can confirm: 80% of parents who double doses do so out of guilt, not ignorance. They feel responsible for the missed dose. But the real failure is the healthcare system that doesn’t hand them a laminated card with the rules on discharge. Simple. Free. Required.
Sandy Crux
23 Dec 2025
Oh, the ‘AAP app’… how quaint. As if a mobile application - designed by overworked bureaucrats who’ve never held a crying toddler at 3 a.m. - could possibly replace clinical judgment. And yet, here we are, outsourcing parental intuition to a beta-tested algorithm. How progressive. How utterly, depressingly, bourgeois.
Michael Ochieng
25 Dec 2025
Just got back from a trip to Nigeria - saw a mom using a clean eyedropper to measure her kid’s malaria meds. No syringe. No app. Just love and a steady hand. This post is great, but let’s not forget: safety isn’t just about tech. It’s about support. And sometimes, it’s just about someone saying, ‘You’re doing fine.’
Jon Paramore
25 Dec 2025
For once-daily meds with t1/2 >12h (e.g., valproate, levetiracetam), the 12-h window is conservative. Pharmacokinetic modeling shows 18-h is acceptable in non-therapeutic-window drugs. But for narrow TI drugs (e.g., phenytoin, digoxin), even 6-h is risky. Always check the drug’s therapeutic index and clearance pathway. Most parents don’t know what ‘renal clearance’ means - that’s the gap.
Jerry Peterson
25 Dec 2025
My wife and I use the AAP app. It saved us when we missed my son’s ADHD med on a flight. We were in Mexico, no pharmacy nearby. The app said ‘skip.’ We did. He was fine. No drama. Just calm. Thanks for making this feel less scary.
Erika Putri Aldana
26 Dec 2025
So... don't double. Got it. But what if you're just really tired? And your kid is screaming? And you think, 'maybe one more ml won't hurt'? That's not ignorance. That's human. And the system doesn't care. It just says 'skip.' Like that fixes anything. 🤦♀️