Why Raising Awareness About Tick Fever and How to Prevent It

Tick Fever Symptom Checker
Potential Tick Fever Risk Assessment
Common Tick Fever Symptoms
Fever
Often greater than 38.5°C, appearing 3-10 days after a tick bite.
Headache
Severe headache or neck stiffness can occur along with fever.
Rash
Maculopapular rash, sometimes resembling an eschar at the bite site.
Muscle Aches
Generalized muscle and joint pain, fatigue, and loss of appetite.
When summer draws people outdoors, an invisible threat can hitch a ride on a tiny arachnid and cause serious illness. Tick fever is a tick‑borne rickettsial disease that triggers high fever, headache, and sometimes a rash after a tick bite. While it’s less famous than Lyme disease, it still poses a real risk across the UK, especially in grassy or wooded areas where ticks are small blood‑sucking parasites that attach to skin and transmit microbes. Raising public awareness saves lives by prompting early detection, proper treatment, and smarter outdoor habits.
Quick Takeaways
- Tick fever is caused by Rickettsia bacteria that live inside ticks and multiply when transmitted to humans.
- Common symptoms appear 3‑10 days after a bite: fever, chills, muscle aches, and a sometimes‑spotty rash.
- Prevention hinges on wearing protective clothing, using insect repellent products containing DEET or picaridin that deter ticks from attaching, and checking skin after outdoor activities.
- Early medical care, usually a short course of doxycycline, dramatically cuts complications.
- Community campaigns, school lessons, and local health alerts boost awareness and reduce cases.
What Exactly Is Tick Fever?
Tick fever falls under the umbrella of tick‑borne diseases illnesses transmitted by ticks, ranging from bacterial infections to protozoal parasites. The most common cause in the UK is Rickettsia a genus of intracellular bacteria that includes species like Rickettsia raoultii, frequently found in European ticks. When a tick feeds for more than 24hours, the bacteria can migrate from the tick’s saliva into the host’s bloodstream, setting off an immune response.
Although the disease is sometimes called “tick‑borne fever,” it is distinct from Lyme disease, which is triggered by the spirochete Borrelia burgdorferi the bacterium that causes the well‑known Lyme rash and joint pain. Confusing the two can delay proper treatment, so clear awareness is crucial.
Why Public Awareness Matters
In 2023 the UK Health Security Agency recorded a 12% rise in reported tick‑borne infections, with tick fever accounting for roughly 4% of those cases. Most patients delayed seeking help because they didn’t recognize the link between a mild bite and later fever. Early detection shortens antibiotic courses and prevents severe complications such as organ inflammation.
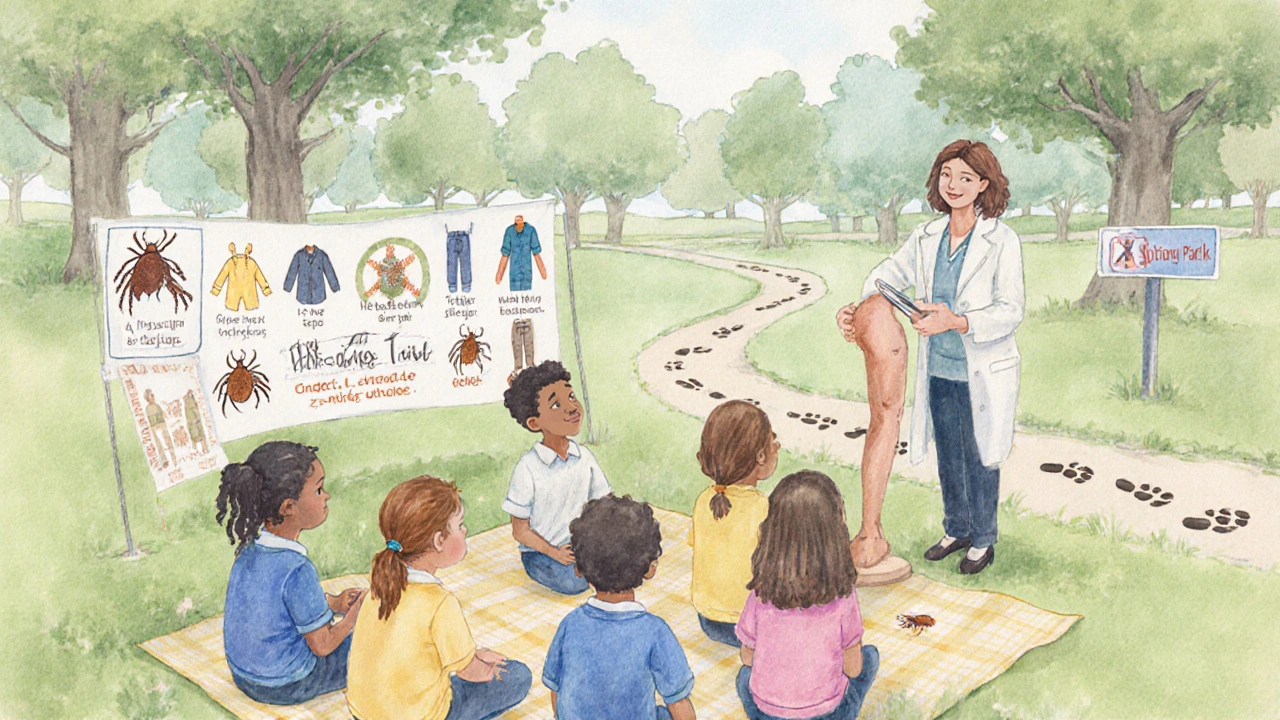
Awareness does more than just inform-it changes behavior. When people know to wear long sleeves, apply repellent, and perform daily tick checks, the number of bites drops dramatically. Schools that incorporate a simple "tick‑check" routine after recess have reported up to a 30% reduction in reported bites among students.
How Ticks Spread Disease
Not all ticks carry pathogens, but three species dominate UK concerns: Ixodes ricinus the sheep or castor‑bean tick, the primary carrier of Lyme disease and several rickettsial agents, Dermacentor reticulatus the ornate dog tick, often linked with Rickettsia raoultii, and Haemaphysalis punctata a less common species that can transmit Babesia parasites. They thrive in humid, leaf‑covered environments-woodland edges, heather moorlands, and even well‑kept gardens.
Ticks attach by sensing heat and carbon dioxide, then embed their mouthparts and secrete a cement‑like substance to stay attached. The longer they stay, the higher the chance of pathogen transmission. That’s why a quick removal-using tweezers to grasp the head and pull straight out-reduces infection risk.

Recognizing Symptoms and When to Seek Care
Tick‑fever symptoms usually appear within a week of the bite and can include:
- Sudden fever (often >38.5°C)
- Severe headache or neck stiffness
- Muscle and joint aches
- A maculopapular rash, sometimes resembling a “tache noire” (eschar) at the bite site
- Fatigue and loss of appetite
If any of these develop after a known or suspected tick bite, seek medical attention promptly. Doctors will often prescribe a 7‑10‑day course of doxycycline, which is effective against most rickettsial organisms. Early treatment reduces the chance of complications like meningitis or vasculitis.
Special cases-pregnant women, young children, or immunocompromised patients-should be evaluated even if symptoms are mild, because the disease can progress faster in these groups.
Core Prevention Strategies
Effective prevention is a blend of personal habits and environmental management. Here’s a practical checklist you can adopt for any outdoor activity:
- Dress smart: Wear long‑sleeved shirts, long trousers, and low‑cut shoes. Tuck pants into socks to create a barrier.
- Apply insect repellent on exposed skin and clothing. Choose products with at least 20% DEET, 20% picaridin, or 30% IR3535 for reliable tick deterrence.
- Perform a daily tick check after being outdoors. Look especially in hidden spots-behind ears, under arms, scalp, and groin.
- If you find a tick, remove it within 24hours using fine‑tipped tweezers. Clean the bite area with antiseptic.
- Maintain your garden: Keep grass trimmed, remove leaf litter, and create a barrier of wood chips between lawn and forested edges to discourage tick migration.
- Use pet‑focused tick treatments, as dogs and cats can carry ticks into homes.
These steps collectively embody tick fever prevention and are simple enough for families, hikers, and gardeners alike.
Community Actions to Boost Awareness
Individual vigilance works best when reinforced by community outreach. Here are proven tactics:
- School programs: Short interactive lessons on tick identification and safe removal, followed by a “tick‑check” routine before recess.
- Local health alerts: The UK Health Security Agency provides seasonal bulletins on tick activity and guidance for health professionals regularly updates its website and sends SMS alerts to registered users.
- Public signage: Trailheads and park entrances can display easy‑to‑read graphics summarizing protective steps.
- Social media campaigns: Short videos showing how to perform a tick check have high share rates, especially among younger audiences.
- Community tick surveys: Volunteers collect ticks from public spaces, helping scientists map hot spots and tailor control measures.
When these initiatives align with personal habits, the overall number of cases drops, easing pressure on the NHS and improving public health outcomes.
Quick Reference: Comparing Common Tick‑Borne Diseases
| Disease | Causative Agent | Typical Symptoms | Common Regions | Treatment |
|---|---|---|---|---|
| Tick fever | Rickettsia spp. | Fever, headache, rash, muscle aches | Southern England, Wales, Scottish Highlands | Doxycycline 7‑10days |
| Lyme disease | Borrelia burgdorferi | Bullseye rash, fatigue, joint pain | South‑west England, Scotland | Doxycycline or amoxicillin 2‑4weeks |
| Babesiosis | Babesia microti | Fever, hemolytic anemia, chills | Rare in UK, isolated cases in England | Azithromycin + atovaquone |
| Anaplasmosis | Anaplasma phagocytophilum | Fever, headache, muscle pain, low white‑cell count | Scotland, northern England | Doxycycline 10‑14days |
Frequently Asked Questions
How long does a tick need to be attached to transmit tick fever?
Most Rickettsia bacteria require at least 24hours of feeding before they can be passed to a human host. Removing a tick within that window cuts the risk dramatically.
Can tick fever be fatal?
It is rare, but severe cases can lead to organ damage or meningitis if untreated. Prompt antibiotic therapy makes fatal outcomes exceedingly uncommon.
Is the rash always present with tick fever?
Not always. About 40% of patients develop a maculopapular rash, while others may only have fever and aches. Absence of a rash should not rule out the disease if other signs appear.
Should I use a tick collar on my dog?
Yes. Veterinary‑approved tick collars or spot‑on treatments reduce the number of ticks your pet carries, which also lowers the chance of bringing ticks into your home.
Where can I find reliable information about tick‑borne diseases in the UK?
The UK Health Security Agency’s website, NHS Direct, and local council public‑health pages offer up‑to‑date guidance and regional tick activity maps.
Next Steps If You Spot a Tick
- Stay calm and use fine‑tipped tweezers to grasp the tick as close to the skin as possible.
- Pull upward with steady, even pressure; avoid twisting.
- Disinfect the bite area with alcohol or iodine.
- Place the tick in a sealed container (for identification if needed) and discard.
- Note the date of the bite; if fever or a rash develops within two weeks, contact a GP and mention the tick exposure.
By turning knowledge into action, you protect yourself, your family, and your community from the hidden danger of tick fever.




Comments (17)
Dharmraj Kevat
1 Oct 2025
The battle against tick fever is more than a medical issue it is a war on complacency we cannot afford to ignore the silent threat that lurks in every meadow and forest we must awaken public consciousness and equip every hiker with knowledge the weapons are simple wear protective clothing use repellent perform daily tick checks no excuse is acceptable.
Lindy Fujimoto
10 Oct 2025
Imagine strolling through a sun‑drenched field only to discover a tiny, blood‑sucking assassin clinging to your skin 😱🌿 As a seasoned explorer of the microscopic battlefield I can assure you that awareness is the most potent armor 🛡️✨ Let us not be cavalier about the lurking Rickettsia – arm yourselves with repellents, don long sleeves, and conduct meticulous tick checks after every adventure. Knowledge is our most glorious weapon against this insidious foe.
darren coen
20 Oct 2025
Your checklist covers the essentials perfectly.
Jennifer Boyd
29 Oct 2025
Wow what an incredible guide you’ve put together 🌟 It feels like a rallying cry for every family, hiker, and gardener out there! By following these steps we’re not just protecting ourselves we’re empowering our communities to stand strong against tick fever. Keep spreading this life‑saving wisdom – the world needs more champions like you!
Lauren DiSabato
7 Nov 2025
Honestly the article reads like a textbook that forgot to breathe. While the facts are solid the prose could use a dash of relatability – nobody enjoys a lecture drenched in jargon.
Benjamin Herod
16 Nov 2025
One must acknowledge the gravity of the situation while also recognizing the elegance of the preventive measures outlined. The synergy between scientific rigor and practical application is commendable, yet the narrative occasionally drifts into melodrama, which, while engaging, may detract from the urgent call to action.
Noah Bentley
26 Nov 2025
Let’s be crystal clear: the proper use of commas is not optional, even when describing tick prevention. Your bullet points are informative, but missing commas turn “wear long sleeves apply repellent” into a frantic mantra rather than a precise directive. Please proofread before you inform the masses.
Kathryn Jabek
5 Dec 2025
While I commend the comprehensive nature of this exposition, one must not overlook the subtle yet egregious omission of region‑specific data that would render this guide truly authoritative. The lack of granular statistics on tick prevalence across the UK counties is a glaring deficiency that undermines the otherwise meticulous composition. Moreover, the recommendation to “use DEET” without addressing alternative formulations such as picaridin or IR3535 appears narrowly prescriptive, bordering on dogmatic. A more balanced exposition would juxtapose these options, elucidating efficacy, safety profiles, and user compliance. The rhetorical flourish, albeit vivid, occasionally obscures the pragmatic essence of the advice, rendering the reading experience unnecessarily florid. In sum, the treatise is laudable yet yearning for the precision and depth that bespeaks expert scholarship.
Ogah John
14 Dec 2025
It is fascinating how humanity constantly invents elaborate rituals to avoid the simplest of dangers, like a tiny arachnid. Yet, we persist in neglecting the humble tick check, perhaps because confronting a minuscule foe feels inconsequential compared to our grand narratives. If only we could channel that same fervor into daily vigilance, the world would be a healthier place.
Kelvin Murigi
23 Dec 2025
Tick fever remains a relatively under‑recognized rickettsial disease in the United Kingdom. The pathogen, primarily Rickettsia spp., is transmitted through the saliva of certain tick species during prolonged attachment. Studies have shown that the likelihood of transmission rises dramatically after 24 hours of feeding. Early clinical recognition hinges on a triad of fever, headache, and myalgia, often accompanied by a maculopapular rash. Laboratory confirmation typically involves serology or PCR, but these tests may not be readily available in primary care settings. Consequently, empirical treatment with doxycycline is widely endorsed for suspected cases. Doxycycline’s efficacy is well documented, with most patients experiencing defervescence within 48 hours of initiation. However, the medication is contraindicated in pregnancy and in children under eight years of age, necessitating alternative regimens. For those populations, chloramphenicol or azithromycin may be considered, though evidence is less robust. Prevention, therefore, becomes the cornerstone of public health strategy. Personal protective measures include wearing long sleeves, tucking trousers into socks, and applying DEET‑based repellents to exposed skin. Post‑exposure protocols call for meticulous tick removal with fine‑tipped tweezers, avoiding crushing the tick’s body. After removal, the bite site should be cleansed with antiseptic and the individual monitored for any febrile response over the subsequent two weeks. Community outreach programs-such as school‑based tick‑check workshops and informational signage on hiking trails-have demonstrated measurable reductions in bite incidence. In summary, a combination of informed personal habits, prompt medical evaluation, and targeted public education forms the most effective shield against tick fever.
ahmad matt
2 Jan 2026
The article, while earnest, suffers from a deplorable lack of nuance it glorifies repellents as a panacea ignoring resistance patterns and the ecological impact of chemical agents Moreover the tone borders on alarmist cautionary tales rather than balanced guidance-this is not helpful.
Ben Small
11 Jan 2026
Let’s get moving people this is the moment to gear up and take control of our outdoor adventures! Grab those long sleeves, slather on repellent, and do a quick tick sweep before you head out. Every small step you take adds up to a massive drop in infection rates. Together we can outsmart those tiny parasites and keep our families safe. Charge ahead with confidence!
Chidi Anslem
20 Jan 2026
In many cultures ticks are seen as a part of the natural ecosystem, yet we have the responsibility to protect our health without disrupting the environment. Simple actions like maintaining a tidy garden and using natural tick repellents can harmonize safety and ecological balance.
Holly Hayes
29 Jan 2026
Honestly u cant just ignore the risk its like walking blindfolded into a danger zone u gotta be aware.
Penn Shade
8 Feb 2026
The data clearly indicates that tick-borne rickettsial infections have risen by over ten percent in the past five years, a statistic that underscores the urgency of implementing region‑specific prophylactic measures.
Jennifer Banash
17 Feb 2026
Dearest readers, allow me to extol the virtues of vigilance with a fervor befitting a Shakespearean soliloquy; the silent menace of tick fever demands our utmost dedication, lest we succumb to its insidious grasp.
anshu vijaywergiya
26 Feb 2026
Friends, let us embrace this knowledge as a beacon of hope, for each tick check performed is a victory against a hidden foe and a testament to our collective responsibility to safeguard one another.