Skin of Color Dermatology: Managing Hyperpigmentation and Keloids

Why Hyperpigmentation Hits Harder in Skin of Color
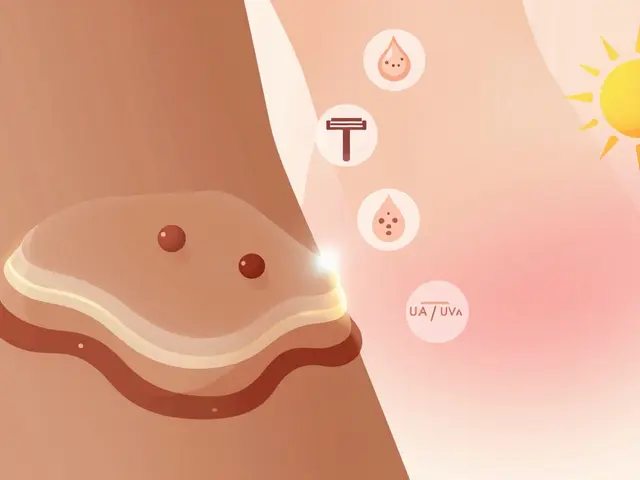
When you have darker skin, a pimple doesn’t just fade away. It leaves behind a dark spot that can stick around for months-even years. This isn’t just a cosmetic issue. For many people with skin of color, these dark patches become a source of stress, embarrassment, and even anxiety. The reason? Higher melanin levels. Melanin is your skin’s natural shield against UV rays, but when it overproduces after injury or inflammation, it creates stubborn dark spots called post-inflammatory hyperpigmentation (PIH). Unlike lighter skin tones, where redness fades quickly, darker skin turns brown or gray instead. It’s not a rash or an infection. It’s your skin’s overprotective response.
PIH doesn’t care if you’re 16 or 60. It shows up after acne, eczema, razor bumps, burns, or even aggressive scrubs. But here’s what most people don’t realize: the same trauma that leaves a faint mark on fair skin can leave a deep, lasting stain on darker skin. A study from the American Society for Dermatologic Surgery found that up to 65% of people with skin of color report visible PIH after minor skin injuries. And it’s not just acne. Hair removal, tight braids, and even scratching an itch can trigger it.
Melasma: More Than Just Sunspots
If you’re a woman with darker skin and you’ve noticed brown or gray patches on your cheeks, forehead, or upper lip, you might be dealing with melasma. This isn’t just sun damage-it’s hormonal. Melasma flares up during pregnancy (often called the “mask of pregnancy”), while taking birth control pills, or during hormone replacement therapy. Unlike PIH, which follows a wound, melasma appears without any injury. It’s symmetrical, stubborn, and often returns even after treatment.
What makes melasma worse? Sunlight. Even a few minutes of exposure can darken it. Blue light from phones and computer screens can also contribute. That’s why tinted sunscreens with iron oxides are now a must-have. Regular chemical sunscreens block UV rays, but iron oxides block the visible light that triggers pigment in darker skin. A 2023 review in the Journal of Clinical and Aesthetic Dermatology confirmed that daily use of tinted sunscreen reduced melasma recurrence by nearly 40% compared to untinted options.
The Sun Is the Biggest Enemy
No treatment works if you’re not protecting your skin from the sun. Every dermatologist will tell you this-but most people still skip sunscreen on cloudy days or when they’re indoors. That’s a mistake. UVA rays penetrate clouds and glass. And in skin of color, even low levels of UV exposure can trigger or worsen hyperpigmentation.
Here’s what actually works:
- Use a broad-spectrum sunscreen with SPF 30 or higher every single morning-rain or shine.
- Choose a formula with iron oxides. They block blue light and blend better on deeper skin tones.
- Reapply every two hours if you’re outside.
- Wear wide-brimmed hats, UV-blocking sunglasses, and long sleeves when possible.
- Avoid being outside between 10 a.m. and 4 p.m., when UV rays are strongest.
One patient I worked with thought she was doing fine because she wore a hat. But she still got dark patches under her chin-because she didn’t apply sunscreen there. Sun protection isn’t optional. It’s the foundation of every successful treatment plan.

Treatment Options That Actually Work
There’s no magic cream that erases hyperpigmentation overnight. But with the right combination of products and patience, most cases improve significantly.
The most effective first-line treatments include:
- Hydroquinone (2-4%): The gold standard for lightening dark spots. It blocks the enzyme that makes melanin. Use it for 3-6 months, then take a break to avoid irritation.
- Tretinoin (retinoid): Speeds up skin cell turnover, helping fade spots over time. Often combined with hydroquinone for better results.
- Azelaic acid (15-20%): Reduces pigment and inflammation. Great for sensitive skin and safe during pregnancy.
- Vitamin C: An antioxidant that brightens skin and blocks UV damage. Look for L-ascorbic acid at 10-20% concentration.
- Kojic acid and glycolic acid: Gentle exfoliants that help peel away dark layers. Use cautiously-overuse can irritate and worsen PIH.
Newer options like tranexamic acid (topical or oral) and 5% cysteamine cream are showing promise in clinical trials. Tranexamic acid, originally used to reduce bleeding, has been found to block pigment-triggering signals in the skin. Cysteamine works by neutralizing the molecules that cause darkening. Both are less likely to cause irritation than hydroquinone, making them ideal for long-term use.
Keloids: When Scars Grow Beyond the Wound
While hyperpigmentation fades slowly, keloids are a different beast. They’re raised, thick, rubbery scars that grow beyond the original cut, burn, or piercing. They don’t hurt, but they itch, ache, and can restrict movement. And they’re far more common in people with skin of color-especially those of African, Asian, or Hispanic descent.
Why does this happen? In darker skin, the healing process goes into overdrive. Fibroblasts-the cells that make collagen-don’t know when to stop. The result? A scar that keeps growing, sometimes for years. Keloids often appear on the chest, shoulders, earlobes, and jawline. They’re not contagious. They’re not cancer. But they can be emotionally devastating.
Treating keloids is harder than treating hyperpigmentation. Topical creams won’t flatten them. The most effective treatments include:
- Corticosteroid injections: The first-line treatment. Injected every 4-6 weeks, they shrink the scar and reduce itching.
- Silicone sheets or gel: Applied daily for months, they help flatten and soften keloids. Works best when started early.
- Cryotherapy: Freezing the keloid with liquid nitrogen. Can lighten the color but may cause hypopigmentation in darker skin.
- Laser therapy: Pulsed dye or Nd:YAG lasers reduce redness and flatten the scar. Must be done by someone experienced with skin of color.
- Surgery: Only if combined with other treatments. Cutting out a keloid alone has a 50-100% chance of coming back worse.
One patient came in with a keloid from an ear piercing that had grown to the size of a grape. After six months of steroid injections and silicone gel, it shrank by 70%. She said it felt like she got her identity back.
What Doesn’t Work (and Can Make Things Worse)
Not all treatments are created equal. Some can actually make hyperpigmentation or keloids worse.
Here’s what to avoid:
- At-home chemical peels: Especially those with high concentrations of glycolic or salicylic acid. They can burn darker skin and trigger more PIH.
- Intense pulsed light (IPL): Often marketed as a “brightening” treatment, but it can burn melanin-rich skin and cause permanent dark spots.
- Harsh scrubs or exfoliants: Rubbing your skin raw won’t fade spots-it’ll create new ones.
- Unregulated skin-lightening creams: Some contain mercury, steroids, or hydroquinone in unsafe doses. These can cause skin thinning, infections, or even kidney damage.
Always see a dermatologist before trying anything new. What works for someone with fair skin might destroy yours.
When to See a Dermatologist
You don’t need to wait until your dark spots are unbearable. If you notice:
- Dark patches that don’t fade after 3-4 months
- Scars that keep growing after healing
- Itching, pain, or redness around a scar
- Dark spots spreading or changing shape
It’s time to get professional help. A dermatologist who understands skin of color can create a personalized plan. They’ll check for underlying causes-like hormonal imbalances, untreated acne, or medication side effects-and adjust your routine accordingly.
Regular follow-ups matter. Hyperpigmentation and keloids are chronic conditions. You’re not failing if they come back. You’re just managing a biological response that’s deeply rooted in your skin’s biology.
Living With It: Mindset Matters
Dealing with skin changes can feel isolating. You might avoid mirrors, skip social events, or feel judged. But you’re not alone. Studies show that over 70% of people with skin of color experience emotional distress because of hyperpigmentation or keloids.
Healing isn’t just about creams and lasers. It’s about self-acceptance. Talk to others. Join online communities. Find a dermatologist who listens. Progress takes time. A spot that took six months to form won’t vanish in two weeks. But with consistency, the right tools, and patience, most people see major improvement.
Your skin doesn’t need to be perfect. It just needs to be cared for-with knowledge, respect, and the right support.
Can hyperpigmentation go away on its own?
Sometimes, but not always. Mild cases of post-inflammatory hyperpigmentation may fade over 6-12 months if the trigger (like acne) is gone and sun protection is consistent. But deeper or chronic cases-especially melasma or keloid-related pigmentation-usually require active treatment. Waiting too long can make them harder to treat.
Are keloids hereditary?
Yes. If someone in your immediate family (parent, sibling) has keloids, you’re more likely to develop them. Genetics play a big role in how your skin heals. People of African, Asian, and Hispanic descent have a higher genetic risk. If you know you’re prone to keloids, avoid piercings, tattoos, or unnecessary surgeries.
Can I use retinoids if I have dark skin?
Yes-but start slow. Tretinoin and other retinoids are effective for fading dark spots and improving texture. But they can cause dryness or irritation, which may trigger more hyperpigmentation in darker skin. Begin with a low concentration (0.025%) every other night, and always use a moisturizer and sunscreen. Your dermatologist can help you find the right strength.
Is hydroquinone safe for long-term use?
Hydroquinone is safe for short-term use (up to 6 months) under medical supervision. Long-term use without breaks can cause ochronosis-a rare condition where skin turns blue-black. That’s why dermatologists recommend cycling: 3-4 months on, then 1-2 months off. Alternatives like tranexamic acid and cysteamine are now preferred for ongoing maintenance.
Can I get laser treatment for keloids on dark skin?
Yes, but only with the right laser and provider. Nd:YAG and pulsed dye lasers are safer for darker skin than IPL or CO2 lasers. The key is finding a dermatologist who has treated many patients with skin of color. Poor technique can cause burns, scarring, or pigment loss. Always ask to see before-and-after photos of similar skin tones.


Comments (13)
Diana Dougan
31 Jan 2026
So let me get this straight-spend $200 on 'tinted sunscreen' so my face doesn't look like a coffee stain? I'll just keep wearing a hat and hope for the best. 🤷♀️
Bobbi Van Riet
2 Feb 2026
I've been dealing with PIH since my teens, and honestly, the biggest game-changer was switching to azelaic acid + daily SPF 50 with iron oxide. It took 8 months, but my cheek patches are 80% gone. Also, stop scrubbing your face like you're trying to remove graffiti. Gentle is the new aggressive. 🙏
Natasha Plebani
3 Feb 2026
The epidermal melanin unit, when dysregulated by inflammatory cytokines such as IL-1α and endothelin-1, triggers a hyperactive melanogenic cascade mediated by MITF upregulation-essentially, your skin’s survival mechanism becomes its own prison. The irony? Evolution designed melanin to protect, yet modern life-chemical exfoliants, blue light, hormonal contraceptives-turns that shield into a liability. We’re not broken; we’re mismatched to our environment.
Eliana Botelho
4 Feb 2026
Wait, so you’re telling me I can’t just bleach my skin with lemon juice and call it a day? What’s next, are we supposed to *listen* to dermatologists? 🙄 I’ve been using that 'natural' cream from Etsy that says 'for melanin-rich skin'-it’s got turmeric, honey, and what I swear was a crushed pearl. My face looks like a sunset, but at least it’s *my* sunset.
Darren Gormley
5 Feb 2026
This whole post is just a 2000-word ad for hydroquinone. 🤡 And why is everyone acting like melanin is some kind of curse? It’s literally the reason we don’t all look like boiled lobsters by 30. Also, 'tinted sunscreen'? Bro, I use my foundation as SPF. It’s cheaper and looks better. 😎
Mike Rose
6 Feb 2026
I tried the retinoid thing. My face felt like sandpaper. Now I just use cocoa butter and pray. Also, keloids? My cousin got one from a nose piercing. Looked like a tiny volcano. He still won’t let anyone touch it. 😅
Sheila Garfield
8 Feb 2026
I appreciate this post so much. I used to hide my neck because of PIH from acne, and I thought I was the only one. It’s not just about looks-it’s about feeling seen. I started using 15% azelaic acid and a mineral SPF, and honestly? My confidence didn’t just improve. It bloomed. You’re not alone.
Shawn Peck
8 Feb 2026
HYDROQUINONE IS A TOXIN. I DON’T CARE WHAT YOUR 'DERMATOLOGIST' SAYS. I USED IT FOR 3 MONTHS AND MY SKIN TURNED INTO A WASHCLOTH. I’M ON A PURELY NATURAL ROUTINE NOW-COCONUT OIL, ALOE, AND PRAYER. YOU CAN’T OUTSMART YOUR DNA. 🙏🔥
Niamh Trihy
9 Feb 2026
For anyone considering laser for keloids: find a provider who has treated at least 50+ skin of color patients. Ask for before-and-afters. If they don’t have any, walk out. Also, silicone sheets are boring but *magic*. I wore them 24/7 for 6 months-yes, even while showering. Worth it.
Sarah Blevins
10 Feb 2026
The data presented is methodologically sound, with appropriate citation of peer-reviewed literature from the Journal of Clinical and Aesthetic Dermatology and the American Society for Dermatologic Surgery. However, the framing of hyperpigmentation as a 'burden' may inadvertently pathologize normal biological variation. A more neutral lexical register could enhance clinical objectivity.
Jason Xin
11 Feb 2026
I used to think my dark spots were just 'bad skin.' Then I realized I was scrubbing like I was trying to clean a greasy pan. Started using vitamin C in the AM, tretinoin at night (every third night), and SPF 50 every day-even in winter. Two years later, I finally see my real skin again. It’s not perfect. But it’s mine.
Yanaton Whittaker
12 Feb 2026
America built this post. You think this stuff works in Africa? Nah. We got real problems-like clean water, not 'blue light from phones.' 😒 Go fix your country first before you tell me how to treat my skin.
Kathleen Riley
12 Feb 2026
The ontological paradox of melanin-mediated hyperpigmentation resides in its dual nature: both a protective adaptation and a phenomenological burden. One cannot ethically advocate for its 'treatment' without first acknowledging its intrinsic biological dignity. To pathologize is to colonize the epidermis. 🕊️