Psoriasis Treatment Options: Plaque, Guttate, and Systemic Therapies Explained
Psoriasis isn’t just a rash. It’s a full-body immune system glitch that turns skin cells into overachievers-multiplying too fast, piling up, and forming thick, red, itchy plaques. For most people, it starts as plaques: raised, scaly patches on elbows, knees, scalp, or lower back. But for others, it hits as tiny, drop-like spots after a sore throat-that’s guttate psoriasis. And when it’s severe, it doesn’t just sit on the skin. It creeps into joints, hearts, and metabolism. The good news? We now have more ways to treat it than ever before. And not all of them are creams you rub on. Some are injections, pills, or even future oral pills that work like biologics without needles.
Understanding the Three Main Types of Psoriasis
Not all psoriasis looks the same. The type you have changes how you treat it.
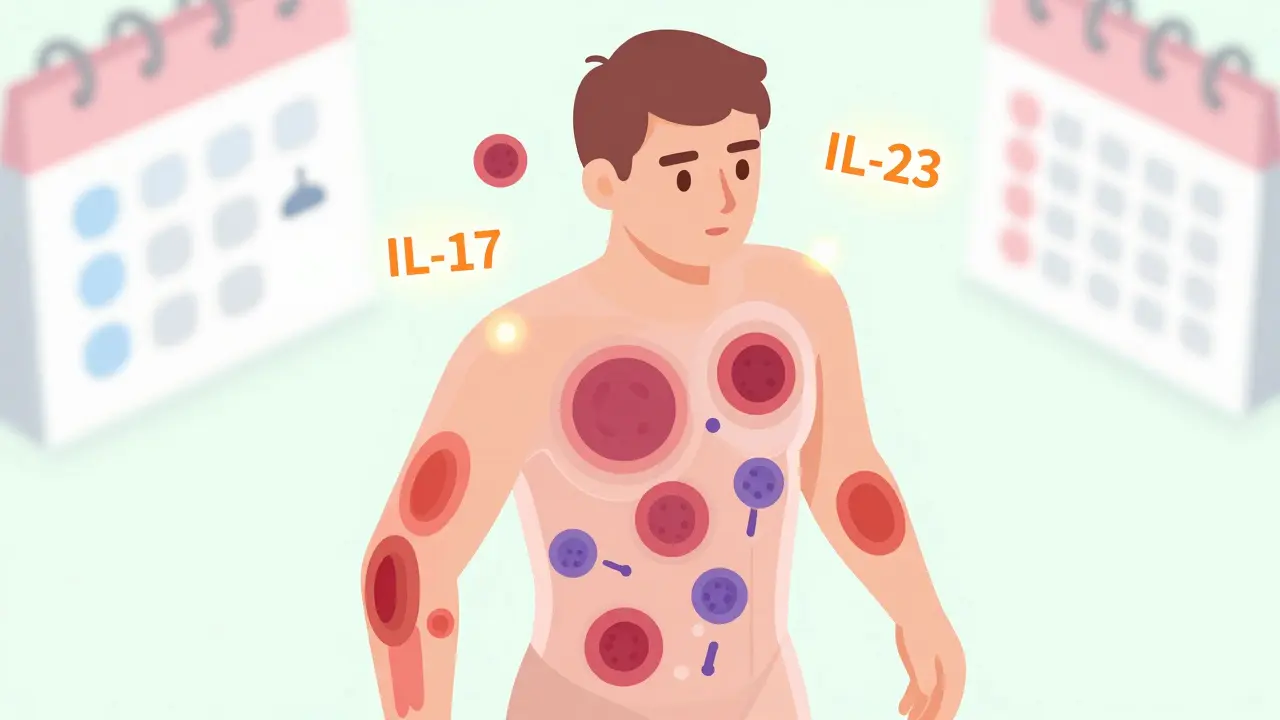
Plaque psoriasis is the big one-80 to 90% of cases. It shows up as thick, silvery scales on red, inflamed skin. These plaques can be painful, crack, bleed, and make daily life hard. They don’t just appear randomly. They often flare after stress, infections, cold weather, or certain medications. The immune system is attacking skin cells like they’re invaders. T-cells and cytokines like IL-17 and IL-23 are running the show.
Guttate psoriasis hits differently. It’s sudden. Often after strep throat, especially in kids and young adults. Instead of big plaques, you get dozens of small, teardrop-shaped spots across the torso, arms, or legs. It can look like a bad case of chickenpox. For many, it clears on its own within weeks. But for some, it sticks around and turns into plaque psoriasis. Treating guttate means tackling the trigger-like antibiotics for strep-and sometimes light therapy or mild topicals.
There are other types-pustular, inverse, erythrodermic-but they’re rare. If you have guttate or plaque, your treatment path usually starts the same: with what’s on the surface. But if it’s not working, you go deeper.
Topical Treatments: The First Line, But Not Enough for Severe Cases
If you’ve got mild psoriasis-less than 5% of your skin covered-topicals are your best bet. They’re cheap, safe, and you can start today.
Corticosteroids are the classic. Strong ones (like clobetasol) work fast. But use them too long, and your skin gets thin, stretchy, or turns white. That’s steroid withdrawal. Dermatologists now recommend using them only 2-4 weeks at a time, then switching to something gentler.
Calcipotriol (a vitamin D analog) is a smart partner. It slows down skin cell growth without thinning skin. You’ll often see it mixed with a steroid in one cream or foam. That combo clears about 35-40% of plaques in 8 weeks. For scalp psoriasis, the foam version works better than lotion-it doesn’t drip, and it sticks to the hairline.
Tapinarof is new. It’s a plant-based cream that calms inflammation without steroids. In trials, 35% of users got 75% clearer skin in 12 weeks. It’s pricier than old-school options, but no skin thinning. Great for long-term use on the face or folds.
But here’s the truth: if your psoriasis covers more than 10% of your body, or it’s on your nails, scalp, or genitals, topicals alone won’t cut it. That’s when you need systemic treatment-drugs that work inside your body.
Systemic Therapies: When Psoriasis Goes Beyond the Skin
When plaques are widespread, painful, or affecting your life-sleep, work, relationships-it’s time for systemic therapy. These aren’t creams. They’re pills or shots that change how your immune system behaves.
Methotrexate has been around for decades. It’s cheap. Taken once a week, it clears about half of moderate-to-severe cases. But it can hurt your liver and lower your blood counts. You need blood tests every few weeks. Not ideal if you drink alcohol or plan to get pregnant.
Cyclosporine works faster-60-70% clear 75% of skin in 12 weeks. But it’s hard on the kidneys. Doctors only use it for short bursts, like 6-12 months, to get you under control before switching to something safer.
Apremilast (Otezla) is an oral pill you take twice a day. It doesn’t suppress your whole immune system. It just tweaks one pathway. About 33% get 75% clearer. It’s safer than methotrexate-no liver or kidney monitoring. But it can cause diarrhea, nausea, and headaches. And it’s expensive: around $7,200 a year before insurance.
Deucravacitinib is newer. A once-daily pill that blocks a specific enzyme (TYK2). In trials, nearly 60% of users hit PASI 75 in 16 weeks. It’s the first oral drug that rivals biologics without the injection. Side effects? Headache, nausea, maybe a slight rise in cholesterol. It’s a game-changer for people who hate needles.

Biologics: Precision Medicine for Psoriasis
Biologics are the most powerful tools we have. They’re made from living cells and target one specific part of the immune system. No guessing. No fishing. Just precision.
TNF inhibitors like adalimumab (Humira) were the first. They work well-78% get 75% clearer. But they’re older. You need shots every other week. And they can increase infection risk. Some people lose effectiveness over time.
IL-17 inhibitors like secukinumab (Cosentyx) are faster. Many see improvement in 2 weeks. They’re great for skin clearance-79% hit PASI 90 (almost 100% clear). But they’re risky if you have Crohn’s or ulcerative colitis. They can make IBD worse. Avoid if you’ve got gut inflammation.
IL-23 inhibitors are the new kings. Guselkumab (Tremfya), risankizumab (Skyrizi), and tildrakizumab (Ilumya) target the root of the problem-IL-23, which drives IL-17. The results? Up to 84-90% of patients hit PASI 90. And they only need shots every 8 to 12 weeks. That’s 4-6 times a year. One patient in Sheffield told me: "I used to dread my biologic appointments. Now I forget when I’m due. I just feel normal."
Real-world data shows risankizumab has the highest persistence rate-78% of people still on it after a year. Guselkumab isn’t far behind. And for scalp and nail psoriasis? IL-23 inhibitors beat everything else. Guselkumab clears scalp psoriasis in 74% of users. Ustekinumab? Only 62%.
Choosing the Right Treatment: It’s Personal
There’s no one-size-fits-all. Your doctor doesn’t just pick the "best" drug. They pick the right one for you.
Here’s how they decide:
- Severity: PASI score over 10? DLQI over 10? That’s moderate-to-severe. Biologics are now first-line, not last-resort.
- Comorbidities: Do you have IBD? Skip IL-17 inhibitors. Got heart disease? Avoid TNF blockers if you’re at high risk. Have diabetes or obesity? You’re more likely to respond well to IL-23 inhibitors.
- Lifestyle: Hate needles? Try deucravacitinib or apremilast. Travel often? Quarterly shots are easier than weekly. Want to get pregnant? Avoid methotrexate and cyclosporine.
- Speed: Need fast relief for a wedding or job interview? IL-17 inhibitors work in weeks. IL-23? Takes 4-8 weeks. TNF? 8-12.
- Cost: Biologics cost $28,000-$34,000 a year. But 85% of insured patients pay $0-$150/month thanks to manufacturer programs. Ask your pharmacy. Don’t assume you can’t afford it.
And here’s a secret: if your first biologic fails, don’t just try another one. Your psoriasis might be a different immune subtype. About 20-25% of people don’t respond to IL-17 blockers because their psoriasis is driven by interferon, not Th17. You need a different approach. Some clinics now do blood tests to find your psoriasis endotype. It’s not standard yet-but it’s coming.
What’s Next? The Future of Psoriasis Treatment
The next five years will change everything.
Oral biologics are already here. Drugs like vunakizumab and imsidolimab are in late trials. They work like injectables but come as pills. One phase 3 study showed 86% got 90% clearer skin. Imagine clearing your skin without needles. That’s the future.
Stopping treatment might be possible. The GUIDE trial is testing whether people who get 100% clear skin with guselkumab can stop entirely and stay clear. Early data suggests yes-for some. This could mean functional cures, not just control.
New topicals are coming too. Creams targeting JAK pathways could hit 50-60% clearance on their own. That means even moderate cases might avoid pills or shots.
And cost? It’s still a barrier. Medicare Part D plans now make you try cheaper drugs first before approving IL-23 inhibitors. But patient assistance programs are better than ever. Most biologic makers give you free doses if you qualify. Talk to your dermatologist’s office-they have specialists who help with this.

Real Stories, Real Results
A 34-year-old teacher in Sheffield tried steroids for 5 years. Nothing worked. Methotrexate gave her nausea and low energy. Then she switched to guselkumab. "In 3 months, my arms were smooth. My scalp? Gone. I started wearing tank tops again. I didn’t realize how much I’d missed that." She pays $120/month thanks to her insurance program.
A 19-year-old student got guttate psoriasis after mono. His doctor gave him light therapy and a mild steroid. Within 6 weeks, the spots faded. He didn’t need anything else.
But not everyone wins. One Reddit user wrote: "I tried secukinumab. Took 4 months. My job interview was in 2 weeks. I cried because I looked like I had burns." Speed matters. If you need fast results, tell your doctor. Don’t wait.
Community advice is real: Use a humidifier in winter. Apply topical steroids under a plastic wrap for stubborn plaques. Avoid alcohol if you’re on methotrexate. Keep a flare journal-stress, diet, infections. You’ll start seeing patterns.
When to See a Dermatologist
You don’t need to suffer. If:
- Your plaques cover more than the size of your palm
- They itch, burn, or hurt daily
- You’ve tried over-the-counter creams for 4 weeks with no change
- Your nails are pitted, thickened, or separating
- Your joints ache or swell
-it’s time to see a dermatologist. Don’t wait. Psoriasis isn’t just skin deep. It’s linked to heart disease, diabetes, depression. Treating it early protects your whole body.
And remember: you’re not alone. The National Psoriasis Foundation’s Biologics Navigator has helped over 100,000 people find the right treatment. Telehealth services now offer consultations in 48 hours. You don’t have to wait months to get help.
Can guttate psoriasis turn into plaque psoriasis?
Yes. About 30% of people who get guttate psoriasis after a strep infection will develop chronic plaque psoriasis within a few years. That’s why even if the spots seem to clear, follow-up with a dermatologist is important. Early treatment can help prevent the transition.
Are biologics safe for long-term use?
Yes, when monitored. Biologics like IL-23 inhibitors have been used for over 6 years in clinical studies with no new major safety signals. The biggest risk is infection-especially TB or fungal infections. That’s why you’re screened before starting. Regular check-ups and blood tests keep you safe. The benefits of clear skin and reduced joint damage far outweigh the risks for most people.
Why do some people not respond to biologics?
Because psoriasis isn’t one disease-it’s several. About 20-25% of people have a different immune driver, like type I interferon, not the Th17 pathway that most biologics target. If your first biologic fails, it’s not that the drug didn’t work-it’s that your psoriasis type needs a different approach. New blood tests can identify your endotype, helping your doctor pick the next best option.
Can I stop taking my psoriasis medication if my skin clears?
Some can. In the GUIDE trial, patients who achieved 100% skin clearance with guselkumab were able to stop treatment and stay clear for months. But this only works for a subset-those who respond deeply and early. Never stop on your own. Talk to your dermatologist. They’ll guide you through a safe taper, if possible.
Is there a cure for psoriasis?
Not yet. But we’re getting closer. With IL-23 inhibitors and emerging oral therapies, many people achieve near-total clearance and stay that way for years. Some may eventually stop treatment without flaring. That’s not a cure, but it’s close enough to feel like one. Research into stopping treatment after early intervention is the most promising path toward true remission.
How do I know if my treatment is working?
Look at your PASI score or your own judgment. If your plaques are thinner, less red, less itchy, and covering less area, you’re on the right track. Most biologics show results in 4-12 weeks. If you see no change after 3 months, talk to your doctor. It might be time to switch. Don’t wait longer-your skin and joints are still under attack.
Next Steps: What to Do Today
If you’re struggling with psoriasis:
- Take a photo of your plaques. Compare it in 4 weeks. Progress is often slow, but it’s there.
- Ask your dermatologist: "Is my psoriasis moderate or severe? Should I be on a systemic treatment?" Don’t assume topicals are enough.
- Request a referral to a psoriasis specialist if your current doctor doesn’t offer biologics. Not all clinics do.
- Call your insurance. Ask: "What biologics are covered? Is there a patient assistance program?" Most manufacturers offer free drugs for qualifying patients.
- Join a support group. Reddit’s r/psoriasis or the National Psoriasis Foundation have real people who’ve been there.
Psoriasis doesn’t define you. But how you treat it? That does. You have more power now than ever before. Use it.






Comments (14)
John O'Brien
26 Jan 2026
Finally someone broke it down without the medical jargon bullshit. I’ve been on guselkumab for 8 months and my scalp is actually visible again. No more baseball cap 24/7. Also, the quarterly shots? Best decision I ever made. Stop letting fear stop you from living.
Also, if you’re on methotrexate and still drinking? You’re not a rebel, you’re just dumb.
Andrew Clausen
27 Jan 2026
The claim that IL-23 inhibitors are superior to IL-17 inhibitors in scalp psoriasis is not supported by head-to-head trials. The PASI 90 data cited is from different studies with different inclusion criteria. The assertion that guselkumab clears scalp psoriasis in 74% of users is misleading without clarifying the baseline severity or duration of treatment. Precision medicine requires precision in data reporting, not marketing spin.
Anjula Jyala
29 Jan 2026
Psoriasis is an autoimmune cascade driven by Th17/IL23 axis. Topicals are palliative. Systemics modulate cytokine networks. Biologics are targeted immunomodulators. Deucravacitinib inhibits TYK2 which is upstream of JAK-STAT. Oral biologics are next-gen. Endotype stratification via transcriptomics is the future. Stop using creams and start treating the immune dysregulation. Your dermatologist should be ordering IL-17/IL-23 biomarkers not just PASI scores.
Also your insurance denies biologics because they’re cheap for pharma and expensive for you. That’s capitalism.
Kirstin Santiago
29 Jan 2026
For anyone reading this and feeling overwhelmed-you’re not alone. I’ve had plaque psoriasis since I was 16. Tried everything. The hardest part wasn’t the skin, it was the shame. I used to wear long sleeves in summer. Now I wear tank tops because I found the right treatment. It took three tries and a lot of tears. But you deserve to feel comfortable in your own skin. Talk to your doc. Ask for a referral. Don’t wait until it’s ‘bad enough.’ You’re worth the effort.
Also, humidifiers are magic. Seriously. Buy one. Your skin will thank you.
Marian Gilan
31 Jan 2026
They don’t want you to know this but biologics are just a cover for Big Pharma’s real agenda. The real cause of psoriasis? 5G radiation + glyphosate in your food + fluoride in the water. The FDA approves these drugs because they’re paid off. Look at the side effects-depression, infections, cancer. They’re not treating you, they’re keeping you dependent. I went off everything and did a 30-day cleanse with turmeric and sunlight. My plaques vanished. No needles. No pills. Just truth.
They’ll call you crazy. Good. The truth always sounds crazy until it’s mainstream.
April Williams
31 Jan 2026
How dare you suggest people with psoriasis should just ‘try’ a biologic? Have you seen the cost? I’m a single mom working two jobs. My insurance says I need to fail three topicals first. That means six months of bleeding, itching, crying in the shower. Meanwhile, my boss thinks I’m ‘gross’ because of my elbows. This isn’t medicine. It’s a class war wrapped in a white coat. And you’re all just nodding along like it’s normal.
My kid has guttate. He’s 8. He’s not getting a $30k/year shot. He’s getting a lotion and prayers.
Harry Henderson
1 Feb 2026
STOP WAITING. I was a mess. Covered. Depressed. Quit the gym. Then I went to a specialist and said ‘I want to be clear in 6 weeks.’ They put me on secukinumab. Six weeks later? I wore shorts. I went swimming. I took a shirt off in front of my girlfriend for the first time in 12 years. This isn’t a chronic disease you live with-it’s a condition you conquer. Get aggressive. Find the right doc. Push. Fight. You’re not broken. You’re just undiagnosed.
suhail ahmed
2 Feb 2026
Man, I’ve been there. Guttate after a fever in Delhi-doctors just said ‘it’ll go.’ Didn’t. Turned into plaque. Tried steroids, then methotrexate, then my cousin’s ayurvedic paste (don’t do that). Finally got on risankizumab. Now I travel for work without hiding my arms. The best part? I can feel my skin again. Not just see it. The warmth. The texture. It’s like getting a part of yourself back. Don’t let anyone tell you it’s ‘just skin.’ It’s your identity. Fight for your skin. You deserve it.
Candice Hartley
3 Feb 2026
I tried everything. Even that weird cream with the plant stuff. 😔 Then I got on deucravacitinib. No shots. Just a pill. My skin cleared in 10 weeks. I cried. 🥹 I didn’t think I’d ever wear a tank top again. Thank you for writing this. I’m not alone. 💙
Conor Flannelly
3 Feb 2026
There’s a quiet dignity in the way modern medicine is learning to listen to the immune system instead of just blasting it. IL-23 inhibitors don’t suppress-they recalibrate. That’s the difference between a hammer and a scalpel. And yet, the most powerful tool remains the patient’s own story-their flare journal, their triggers, their sleep, their stress. Science gives us weapons. But the war is fought in the quiet hours, in the bathroom mirror, in the choice to keep trying. We’re not just treating disease. We’re restoring personhood.
Conor Murphy
4 Feb 2026
My brother had psoriasis for 15 years. He stopped treatment because he thought it was ‘just skin.’ Then he got arthritis in his knees. Now he’s on guselkumab and his joints feel like they did in college. He says he wishes he’d started sooner. Don’t wait until it’s in your joints. Don’t wait until you’re embarrassed to hold your kid’s hand. Do it now. Your future self will thank you.
Paul Taylor
5 Feb 2026
I’ve been on apremilast for two years and I’ve got to say it’s not perfect but it’s the only thing that didn’t make me feel like a lab rat. The nausea in the beginning was rough but I pushed through. Now I take it with food and a banana and it’s fine. I don’t get 100% clear but I get 70% and that’s enough to go to the beach. I don’t care if it’s not the ‘best’ drug. It’s mine. And I’m not going to spend $30k a year just to look ‘perfect.’ I’m just trying to live. Also, if you’re on biologics and you get a cold? Don’t panic. You’re not going to die. You’re just more likely to be sick for a week. That’s it. Your immune system isn’t gone. It’s just dialed down. You’re not a zombie. You’re a human with a smart treatment plan.
Desaundrea Morton-Pusey
6 Feb 2026
Of course the FDA approves these drugs. They’re owned by the same people who own the hospitals and the insurance companies. They want you sick and dependent. Why else would they make you try topical steroids first? That’s not medicine, that’s a money trap. And don’t even get me started on the ‘patient assistance programs.’ They’re designed to make you jump through hoops so you give up. They don’t want you cured. They want you paying. Always.
Murphy Game
8 Feb 2026
They’re lying about the safety data. Look at the VAERS reports. Look at the lawsuits. Biologics cause autoimmune disorders in other systems. Lupus. MS. My cousin got it after Humira. They bury the data. They call it ‘rare.’ But it’s not rare if you’re one of the ones. And now they’re pushing oral versions? So you can take it at home? So they don’t have to monitor you? So you die quietly? I’m not taking it. I’d rather live with the plaques than die from the cure.