Levothyroxine Generics: When to Monitor TSH After Switching Products

Switching between different brands of generic levothyroxine is common-over 89% of prescriptions in the U.S. are filled with generics. But if your TSH level suddenly spikes after a switch, you’re not imagining it. The question isn’t whether switching matters-it’s who it matters for, and when you actually need to check your TSH.
Why Levothyroxine Is Different
Levothyroxine isn’t like taking a generic ibuprofen. It’s a narrow therapeutic index (NTI) drug, meaning tiny changes in blood levels can cause big effects. Your body needs just the right amount of thyroid hormone to keep your metabolism, heart rate, and energy stable. Too little? You feel tired, gain weight, and get cold. Too much? Your heart races, you lose weight, and you feel anxious. The target TSH range for most adults is 0.4 to 4.0 mIU/L. For older adults or those with heart disease, it might stretch up to 6.0 mIU/L. Even a 10% change in absorbed dose can push you outside that range.The FDA says generic levothyroxine products are bioequivalent. That means, on paper, they deliver the same amount of hormone as the brand name. But bioequivalence standards for most drugs allow a 80-125% range in absorption. For NTI drugs like levothyroxine, experts argue that range should be tighter-closer to 90-111%. The FDA hasn’t changed the rule, even though the American Thyroid Association asked them to in 2014. So, while the math says they’re the same, real bodies don’t always react the same way.
The Big Study That Changed Things
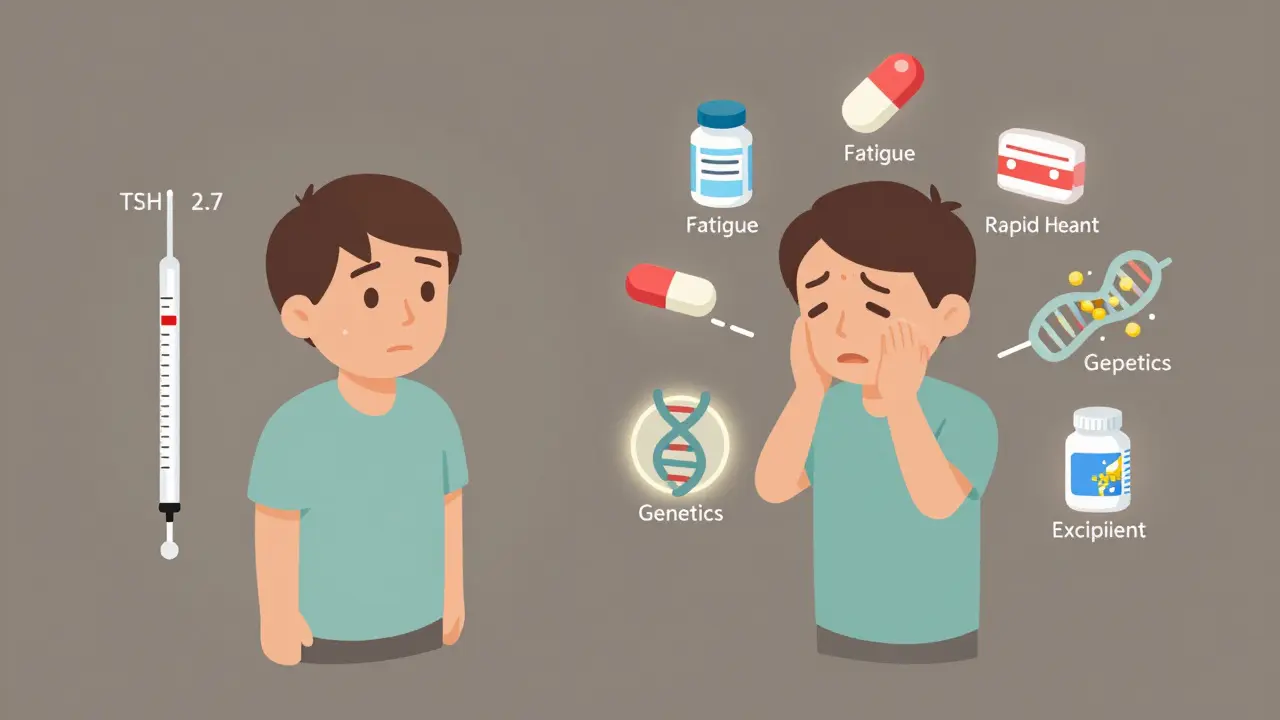
In February 2022, a massive study published in JAMA Internal Medicine looked at over 15,000 patients who switched between generic levothyroxine products. The researchers compared TSH levels before and after the switch. They found no meaningful difference. The average TSH was 2.7 mIU/L for both groups-switchers and non-switchers. The percentage of patients with normal TSH? 64.3% vs. 63.8%. The number with dangerously high or low TSH? Nearly identical. This wasn’t a small trial. It was matched-pair analysis, controlling for age, dose, and medical history. The conclusion: for most people, switching generics doesn’t mess with thyroid control.This study didn’t just sit on a shelf. The FDA updated its labeling in January 2024 to say: “For most patients, switching between different levothyroxine products does not require additional TSH monitoring beyond routine follow-up.” That’s a big shift. It’s based on real-world data, not theory.
Who Still Needs Monitoring
The “most patients” part is key. Some people are more sensitive. If you fall into one of these groups, check your TSH 6-8 weeks after any switch:- You have thyroid cancer and are on suppressive therapy (TSH goal below 0.1 mIU/L)
- You’re pregnant or planning to be
- You have heart disease, especially atrial fibrillation or heart failure
- Your TSH has been unstable before-fluctuating even on the same brand
- You’ve had symptoms after switching before (fatigue, palpitations, weight shifts)
These groups make up a small portion of users-maybe 10-15%. But for them, even a 5% difference in absorption can be dangerous. A 2021 Dutch study found that patients on doses over 100 mcg who switched brands had a 63% chance of abnormal TSH levels. That’s not a fluke. It’s a signal.

What Patients Are Saying
Online forums like Reddit’s r/Hashimotos are full of stories. One user, ThyroidWarrior89, switched from Mylan to Teva and saw their TSH jump from 1.8 to 7.2 in eight weeks. They had to increase their dose by 12.5 mcg. Another, HypoNoMore, switched between three generics over two years with zero TSH changes. Both are real. Both are valid.The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) tracked over 1,200 reports of side effects after switching. The most common? Fatigue (327 cases), palpitations (289), and weight changes (215). That’s not nothing. But it’s also not the majority. Only about 18.7% of patients in one survey reported noticeable symptoms. That means 81% didn’t feel a thing.
What Doctors Are Doing Now
Guidelines are changing fast. The American Association of Clinical Endocrinologists (AACE) and the American Thyroid Association (ATA) used to say: monitor after every switch. Now? Their 2023 updates say: don’t bother unless you’re high-risk. Kaiser Permanente dropped routine monitoring for stable patients in 2023 after studying 18,432 people. The Veterans Health Administration still requires TSH testing within 60 days of a switch-because they manage complex cases. But most private practices? They’re following the new evidence.The UK’s NHS says: if you feel off after a switch, get tested. If you feel fine, keep going. No need to test unless there’s a reason.
Why the Confusion Still Exists
There are three reasons this debate won’t go away:- Excipients matter-the fillers, dyes, and binders in pills vary between manufacturers. Some people are sensitive to lactose, corn starch, or dyes. A 2022 BMJ Open study found 1.7% of switchers had reactions tied to these ingredients.
- Genetics play a role-a small group (about 0.8%) have a gene variant (DIO2) that affects how their body converts T4 to active T3. These people may need consistent dosing.
- Psychological factors-if you believe a switch will mess you up, you’re more likely to notice symptoms. Placebo and nocebo effects are real in thyroid care.
That’s why some doctors still recommend sticking to one brand. It’s not because generics are unsafe. It’s because for a small group, consistency reduces uncertainty.
What You Should Do
Here’s your simple action plan:- If you’re stable, feel fine, and have no high-risk conditions: don’t get a TSH test after a switch. Wait for your next routine check-up.
- If you’re in a high-risk group (cancer, pregnancy, heart disease): get a TSH test 6-8 weeks after the switch.
- If you’ve had symptoms after switching before: track your dose and brand. Keep a note in your phone or journal. Tell your doctor if you feel different.
- If you’re worried: ask for a TSH test. No doctor should dismiss your concern. You’re not being difficult-you’re being proactive.
Don’t let pharmacy policies dictate your care. If your pharmacist switches your pill without telling you, call your doctor. Ask if you’re in the group that needs monitoring. Most won’t. But if you are, you deserve to know.
The Bottom Line
For 88-92% of people taking levothyroxine, switching between generic brands is safe. No extra TSH tests needed. The science supports it. The FDA says it. The biggest health systems are moving that way.But for the 8-12% who are sensitive-whether because of genetics, excipients, or past reactions-consistency matters. That’s not a flaw in generics. It’s human biology.
The goal isn’t to stop generic substitution. It’s to stop blanket rules. Monitoring shouldn’t be automatic. It should be targeted. Smart. Personal.
Know your risk. Know your body. And if something feels off-get it checked. You’re not overreacting. You’re taking control.





Comments (12)
Marc Bains
31 Jan 2026
Look, I get why people freak out about switching generics. I’ve been on levothyroxine for 12 years and switched brands six times. Felt fine every single time. But I also know people who swear their life fell apart after a pharmacy swap. The science says it’s fine for most. But medicine isn’t just stats-it’s lived experience. If you feel different, get tested. No shame in that.
kate jones
1 Feb 2026
The FDA’s 80–125% bioequivalence window is outdated for NTI drugs like levothyroxine. The American Thyroid Association’s 2014 request to tighten it to 90–111% was scientifically sound. Until that changes, clinicians should treat brand switches as potential perturbations-not inert events. Especially in vulnerable populations: pregnant patients, those with cardiac arrhythmias, or on suppressive therapy post-thyroidectomy. Monitoring isn’t overcautious-it’s precision medicine.
Kelly Weinhold
2 Feb 2026
I switched from Teva to Mylan last year and felt like a zombie for two weeks-total brain fog, weight gain, zero motivation. I was about to quit my job. Got my TSH checked and it was 8.1. My doc upped my dose by 12.5 mcg and I’m back to hiking and baking sourdough. So yeah, the study says ‘most people’ are fine. But what about the 12% who aren’t? We’re not outliers-we’re the reason guidelines need nuance. Don’t dismiss our stories just because they’re not in the data.
Kimberly Reker
2 Feb 2026
My mom’s been on Synthroid for 20 years. Her pharmacist switched her to a generic without telling her. She started having heart palpitations and panic attacks. Went to her endo-TSH was off the charts. They switched her back and she’s fine now. Point is: pharmacists aren’t doctors. Just because a pill looks the same doesn’t mean it acts the same. Always know what you’re getting. Ask for the brand if you’re sensitive. It’s your body.
Eliana Botelho
3 Feb 2026
Oh please. The whole ‘some people are sensitive’ thing is just placebo effect wrapped in thyroid anxiety. People read Reddit stories and then their brain starts manufacturing symptoms. I switched between seven different generics over five years. TSH never budged. My energy? Always perfect. If you’re blaming your laziness on levothyroxine, maybe you need a therapist, not a blood test. Stop giving pseudoscience oxygen.
Rob Webber
4 Feb 2026
This whole ‘monitor only if high-risk’ thing is a corporate lie. Pharma companies don’t want you testing after every switch because it costs them money. The FDA’s lazy. The AMA’s lazy. They’re letting pharmacies cut corners and calling it ‘evidence-based.’ I’ve seen patients crash into thyroid storm because no one checked TSH after a switch. This isn’t ‘personalized medicine’-it’s negligence dressed up as science.
Lisa McCluskey
6 Feb 2026
My TSH stayed stable through three switches. I’m in the 80%. But I know someone who had a 400% spike after one swap. So I get why doctors still test. Maybe the rule should be: if you’ve ever had a bad reaction, assume you’re in the 12%. No need to test everyone, but don’t assume everyone’s fine. Listen to the person, not just the study.
Claire Wiltshire
6 Feb 2026
Thank you for this thoughtful, well-referenced breakdown. It’s refreshing to see a post that doesn’t reduce a complex medical issue to binary opinions. The distinction between population-level data and individual physiological variation is critical. I’ve shared this with my patients who are anxious about switching. The action plan you provided is clear, compassionate, and clinically sound. Keep doing this kind of work.
Mike Rose
8 Feb 2026
generic pills are all the same bro. why you actin like your thyroid is a fancy watch? just take the damn pill and stop overthinkin. my cousin switched 5 times and still runs marathons. you guys need to chill.
Niamh Trihy
8 Feb 2026
Interesting that the UK’s NHS takes a symptom-led approach. In Ireland, we do the same. If you’re clinically stable and asymptomatic, no routine testing. But if you report fatigue, palpitations, or unexplained weight changes after a switch, we test. It’s pragmatic. The data supports it. And it avoids unnecessary healthcare costs. Still, I always document the brand and lot number-just in case.
Sazzy De
9 Feb 2026
My doctor told me to just wait for my next checkup after switching. I did. Felt fine. But I kept a note in my phone: ‘Teva → Mylan, April 2023.’ Just in case. Sometimes the little things matter more than the big studies.
Natasha Plebani
11 Feb 2026
The real issue here isn’t bioequivalence-it’s the epistemological gap between population statistics and embodied experience. The study measures TSH, but it doesn’t measure fatigue, anxiety, or the quiet dread of waking up feeling like your body isn’t yours anymore. Science tells us ‘most people’ are fine. But for the ones who aren’t, ‘most’ doesn’t comfort. It isolates. We need a framework that doesn’t reduce human physiology to averages, but honors variability as biological truth-not noise.